A multicenter phase 1/2a randomized, double-blinded, placebo-controlled clinical trial has been conducted recently to evaluate the safety, reactogenicity, and immunogenicity of a non-replicating adenovirus-based vaccine, namely Ad26.COV2.S against severe acute respiratory coronavirus 2 (SARS-CoV-2) infection.
The findings demonstrate that the vaccine is mostly safe for human use and is capable of inducing robust immune responses. The study is currently available on the medRxiv* preprint server.
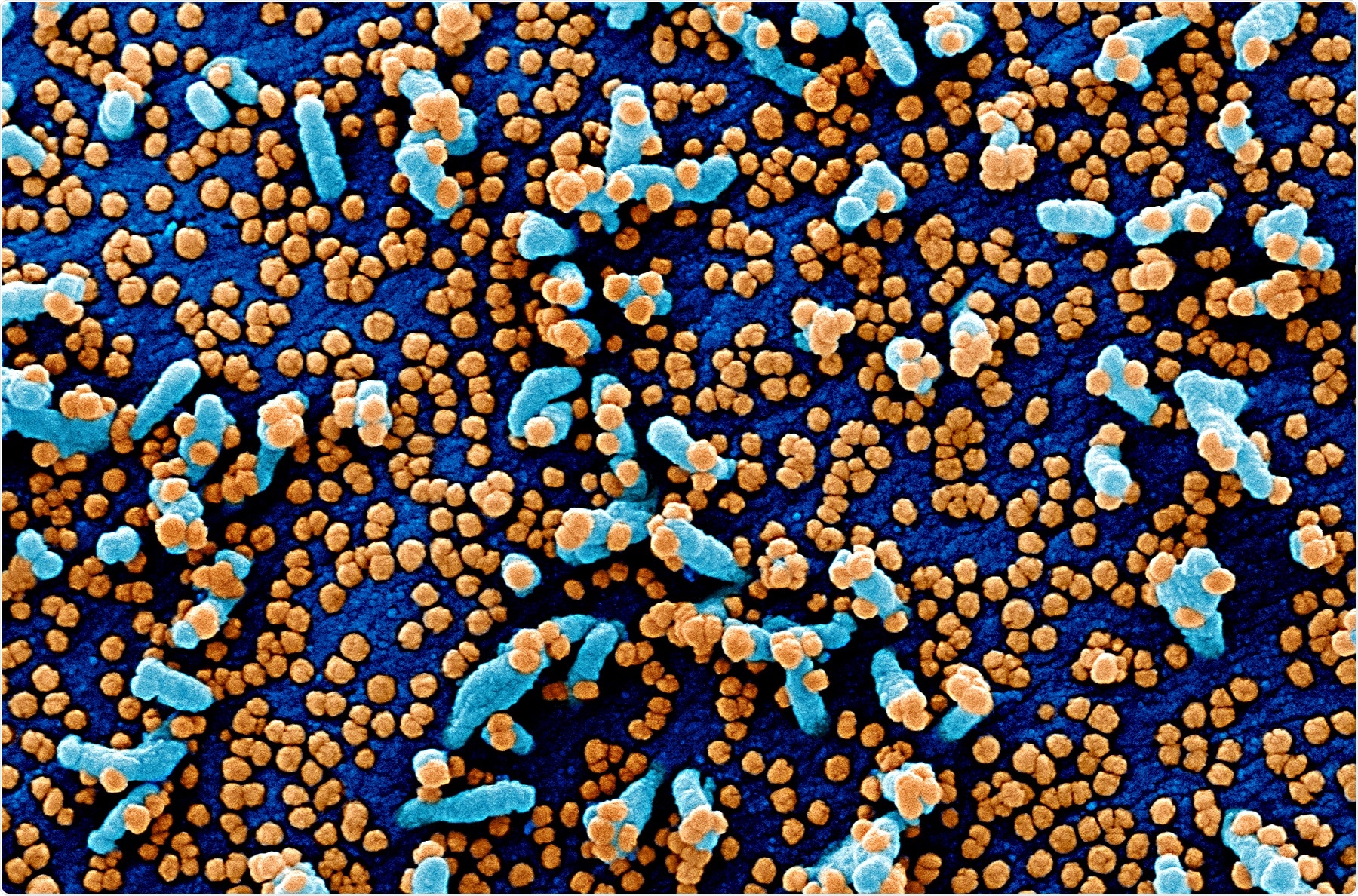
Colorized scanning electron micrograph of a VERO E6 cell (blue) heavily infected with SARS-COV-2 virus particles (orange), isolated from a patient sample. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Since its emergence in December 2019, SARS-CoV-2 has infected over 33.24 million individuals and claimed nearly one million lives worldwide. To contain the rapid spread of SARS-CoV-2, the causative pathogen of coronavirus disease 2019 (COVID-19) pandemic, several vaccines are currently under different stages of preclinical and clinical trials.
In the current study, the safety and efficacy of Ad26.COV2.S vaccine has been assessed. The vaccine is based on non-replicating adenovirus serotype 26 vector, a well-tolerated, highly immunogenic viral vector used previously for Ebola, Zika, and human immunodeficiency virus (HIV) vaccines.
In preclinical studies, the vaccine has been shown to induce strong immune responses in monkeys. Immunization of monkeys with the vaccine results in undetectable viral load in the bronchoalveolar lavage and induction of neutralizing activity in serum.
Similar efficacy of the vaccine has also been observed in a Syrian golden hamster model of severe COVID-19. These promising findings encourage scientists to conduct a phase 1/2a clinical trial.
Current study design
In the current clinical trial, a single-dose vaccination regimen was followed with 5x1010 or 1x1011 viral particles per vaccination in adults belonging to two age groups (18 – 55 years (group 1a and 1b; n = 402) and ≥65 years (group 3; n = 394)). The safety and efficacy of the vaccine were assessed after 4 weeks of vaccination.
Important observations
The study participants received the vaccine (5x1010 or 1x1011 virus particles per vaccination) through intramuscular injections. Solicited and unsolicited adverse events were recorded for 7 and 28 days after vaccination, respectively.
Safety-related findings
About 58% and 27% of participants from groups 1 and 3 showed solicited local adverse events, whereas solicited systemic adverse events were detected in 64% and 36% of participants, respectively. Pain at the site of injection was the most common local adverse event, and fatigue, headache, and myalgia were the most frequently observed solicited adverse events. A mild-to-moderate intensity fever was observed in 19% and 4% of participants from groups 1 and 3, respectively. However, the fever mostly resolved within 1 to 2 days.
Although none of the participants discontinued the trial due to adverse side-effects, there were two severe adverse events recorded. One participant had hypotension; however, this effect is not related to vaccination as the participant had a history of hypotension. Another participant with fever was hospitalized as a suspected case of COVID-19; however, the fever resolved within 12 hours.
Serological findings
The neutralizing antibody titers against SARS-CoV-2 was detected using wild-type virus neutralization assay (wtVNA). The seroconversion rate, which describes the rate of transition from seronegative to seropositive condition, with both low and high doses (5x1010 or 1x1011 viral particle) of vaccination, was found to be 92% (average antibody titer for low dose: 214; average antibody titer for high dose: 243) in the group 1a at day 29. Similarly, the seroconversion rates of 15 participants from the group 3 were found to be 100% and 83% for the 5x1010 and 1x1011 viral particle dose levels, respectively (average antibody titer for low dose: 196; average antibody titer for high dose: 127).
For antibodies developed against the viral spike protein, the seroconversion was measured using ELISA, and the antibodies were detected in 99% and 100% of participants from groups 1a and 3, respectively. The average antibody titers for the low and high doses were 528 and 695, respectively, in group 1a; whereas, the average antibody titers for the low and high doses were 507 and 248, respectively.
Regarding T cell-mediated immune responses after 14 days of vaccination, spike protein-specific CD4+ T cell-mediated Th1 immune responses were observed in 80% and 83% of a subclass of participants in groups 1a and 3, respectively. However, no Th2 immune responses were observed. In both groups, a strong CD8+ immune response was observed.
Overall, the current study observations indicate that the vaccine is safe to use at any age, and a higher vaccine dose is associated with higher reactogenicity. However, the reactogenicity was relatively lower in older adults.
Regarding the immune response, the vaccine is capable of inducing strong neutralizing antibody response and T cell-mediated immune response among the entire study cohort. Based on these observations, a phase 3 trial of the vaccine has been initiated in the US. Moreover, another trial has been planned to evaluate the efficacy and durability of the adaptive immunity of a two-dose regimen of the vaccine.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
medRxiv preprint server. 2020. Sadoff J. Safety and immunogenicity of the Ad26.COV2.S COVID-19 vaccine candidate: interim results of a phase 1/2a, double-blind, randomized, placebo-controlled trial. https://www.medrxiv.org/content/10.1101/2020.09.23.20199604v1
- Peer reviewed and published scientific report.
Sadoff, Jerald, Mathieu Le Gars, Georgi Shukarev, Dirk Heerwegh, Carla Truyers, Anne M. de Groot, Jeroen Stoop, et al. 2021. “Interim Results of a Phase 1–2a Trial of Ad26.COV2.S Covid-19 Vaccine.” New England Journal of Medicine, January. https://doi.org/10.1056/nejmoa2034201. https://www.nejm.org/doi/10.1056/NEJMoa2034201.