Our ability to regulate body temperature and keep our bodies from becoming dehydrated declines as we get older. New research published today in The Journal of Physiology improves our understanding of the relation between temperature regulation and dehydration.
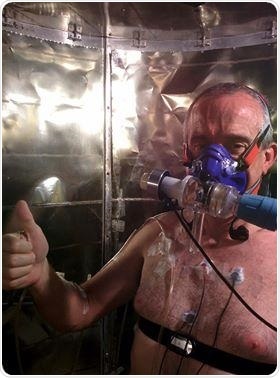
Participant seated within the calorimeter, which measures how much heat his body is losing
This research can help us to better tailor strategies for managing both body temperature regulation and hydration during heat exposure in older adults. For example, because of reductions in thirst and our ability to preserve body fluid, as we age, we may require more frequent reminders to drink water during work in the heat or during heatwaves.
Exercise, especially when performed in a hot environment, exposes the body to heat stress, which causes body temperature to increase.
In these situations, we rely on sweating to help remove heat from the body and prevent continued rises in body temperature, which may increase the risk of heat-related illness or injury (such as heat stroke).
However, prolonged sweating can cause too much fluid to be lost from the body. Unless the person drinks water or a sports drink, this can lead to dehydration. Dehydration also reduces the volume of circulating blood and increases the blood's salt content.
Not only does dehydration make our mouths dry and make us want to drink water, it also impacts the regulation of body temperature. When we become dehydrated, we sweat less and, as a result, lose less heat and become less able to cool the body.
While this can be disadvantageous to regulating body temperature, these adjustments limit further fluid losses and slow the rate of dehydration. Thus, our body’s response to dehydration acts to balance the body’s fluid and temperature regulatory needs.
Until recently, however, our understanding of the effects of dehydration on body temperature regulation came primarily from studies conducted in young adults.
Dehydration did not reduce heat loss or increase body temperature in the older adults during exercise. At first glance this seems like a beneficial response. However, this meant that the older adults did not attempt to adjust the rate of sweat loss to prevent further dehydration. As a result, they experienced greater strain on the heart as evidenced by a more pronounced increase in heart rate compared to younger men.
Previous literature indicates that as we age, our body responds less efficiently to dehydration, and some have suggested that this is due to an impaired ability of the body to ‘sense’ increases in salt levels in the blood (i.e. lack of water) that would normally trigger thirst and drinking.
Since the reduction in sweat rate during dehydration is beneficial for reducing fluid loss, researchers at the Human and Environmental Physiology Research Unit at the University of Ottawa reasoned that a reduced sensitivity to elevated blood osmolality (which is a measure of the bloods saltiness) may also explain the blunted effect of dehydration on heat loss and body temperature regulation in older adults during exercise in the heat.
To evaluate this hypothesis, the research group had young and older men perform exercise in the heat. Before exercise, blood salt content was increased artificially by giving them infusions of saline (salt water).
The participants performed the exercise in a device called a whole-body direct calorimeter, which precisely tracks the amount of heat lost from the entire body, which is caused by increases in sweating and blood flow to the skin.
The primary finding of the study was that, in contrast to young adults, the regulation of body temperature in the older adults was not influenced by increases in the saltiness of the blood.
Less efficient regulation of body temperature and hydration status are thought to contribute to the increased risk of mild (e.g. heat exhaustion) and severe (e.g., heat stroke) heat-related injuries as well as adverse heart problems experienced by older adults during heat stress, such as during occupational work in the heat (e.g., electrical utilities, construction) or in their homes/communities during heatwaves.
Since the young and older adults were physically active without any overt chronic health conditions it is difficult to know whether our findings translate to more sedentary individuals or those with common age-related chronic diseases such as Type 2 diabetes.
Given that common age-related chronic health conditions such as type-2 diabetes are associated with less efficient regulation of body temperature and hydration status, future research should be conducted to see whether our findings translate to or are exaggerated in those populations. While our research design allowed us to test the independent effect of osmolality on heat loss, the effect of reduced blood volume (termed hypovolemia) on sweating in older adults is currently unknown.
Robert Meade, first author