The coronavirus pandemic first emerged in Wuhan City in China in December 2019. From there, it has spread to 188 countries and territories and has affected more than 37 million people. As the pandemic evolves, the symptoms that were reported in the past, such as fever, cough, and difficulty of breathing, have expanded with further clinical manifestations now being reported.
Recently, clinicians report additional symptoms, which hint the involvement of other organs in the body, including the heart and brain.
Many hospitalized patients with coronavirus disease (COVID-19) manifest neurological symptoms such as stroke and encephalitis, among others. This has baffled clinicians on how the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) affects the brain, particularly the peripheral vasculature.
Now, a new study published on the preprint server bioRxiv* sheds light on the mechanism behind brain involvement in the COVID-19 pandemic. A team of researchers at the Krembil Research Institute and the University of Toronto in Canada aimed to understand further the potential mechanisms underlying SARS-CoV-2 tropism for brain vasculature to see how infection occurs in the brain.
The study
The team wanted to determine the cause of why COVID-19 patients experience neurological symptoms, including strokes and encephalitis, a potentially deadly inflammation of the brain. A recent study has also shown that a third of hospitalized patients affected by COVID-19 exhibited acute cerebrovascular events, including ischemic and hemorrhagic strokes, impaired consciousness, and muscle injury, which were even more common in patients with severe illness.
This new study involved constructing a molecular atlas of the expression patterns of the SARS-CoV-2 viral entry-associated genes, including receptors and proteases, and SARS-CoV-2 interaction partners in human and mice brains.
To arrive at the study findings, the researchers examined the expression patterns of the virus on the brain. They found that a distinct expression pattern of the cathepsins B (CTSB) and -L (CTSL), which can substitute for the angiotensin-converting enzyme 2 (ACE2) receptor TMPRSS2, in the human vasculature. They also found that the CTSB is mainly expressed in the brain blood vessels, and CTSL is seen predominantly in the peripheral blood vessels.
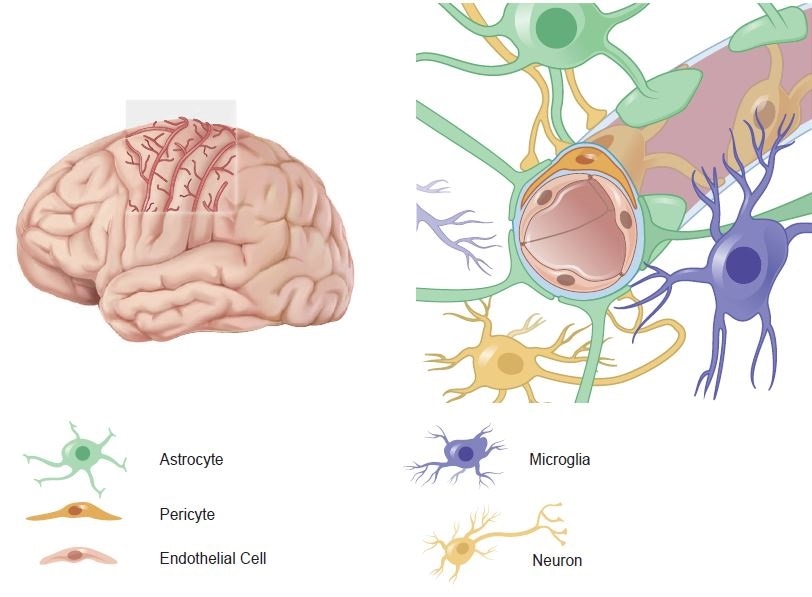
Expression of SARS-Cov-2 entry associated genes in human adult and fetal brain endothelial- and perivascular cells a Scheme illustrating brain blood vessels running within cortical sulci (left). The neurovascular unit (NVU) is composed of endothelial cells and of perivascular cell types such as pericytes, astrocytes, neurons, and microglia.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
To confirm the findings, the team examined the mechanism in the protein level in the Human Protein Atlas and through the use of immunofluorescence staining.
Further, the team confirmed that the same findings were seen in the fetal brain, suggesting a developmentally established SARS-CoV-2 entry machinery in the human blood vessels or vasculature.
"At both the adult and fetal stages, we detected a distinct pattern of SARS-CoV-2 entry associated genes' transcripts in brain vascular endothelial cells and microglia, providing a potential explanation for an inflammatory response in the brain endothelium upon SARS-CoV-2 infection," the researchers explained in the study.
Also, CTSB was expressed in adult and fetal brain endothelial cells, with genes and pathways involved in innate immunity and inflammation, blood-brain-barrier permeability, angiogenesis, coagulation, and vascular metabolism. These findings highlight the role of brain endothelial cells in developing neurological symptoms in some COVID-19 patients.
"Our study serves as a publicly available single-cell atlas of SARS-CoV-2 related entry factors and interaction partners in human and mouse brain endothelial- and perivascular cells, which can be employed for future studies in clinical samples of COVID-19 patients," the team concluded in the study.
Brain fog in COVID-19 survivors
The involvement of the brain in the disease process of COVID-19 has been seen in some patients who have already recovered from the infection. In a New York Times article, patients describe neurological symptoms amidst their battle against the coronavirus infection.
One patient described that after recovering from COVID-19, she experienced confusion and memory loss, even forgetting her car in the parking lot. Another patient recalled losing all memory of his 12-day vacation in Paris, even though the travel was just a few weeks prior.
A nurse also experienced forgetfulness after recovering from the infection. The nurse forgets routine treatments and tests, even terminologies that were always used in the past.
Many patients who went ill with COVID-19 experience brain fog, which included troubling cognitive symptoms that include confusion, memory loss, dizziness, problems in concentration, and trouble remembering everyday words.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Sources:
Journal reference: