Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel betacoronavirus that emerged in December 2019 in Wuhan, China, and is the cause of coronavirus disease 2019 (COVID-19) pandemic. It has affected over 38 million people worldwide, with over 1 million fatal cases to date. The most common symptoms involve fever, cough, and cold; severe symptoms may be difficulty breathing (dyspnoea) or shortness of breath, chest pain or pressure, and loss of speech or movement.
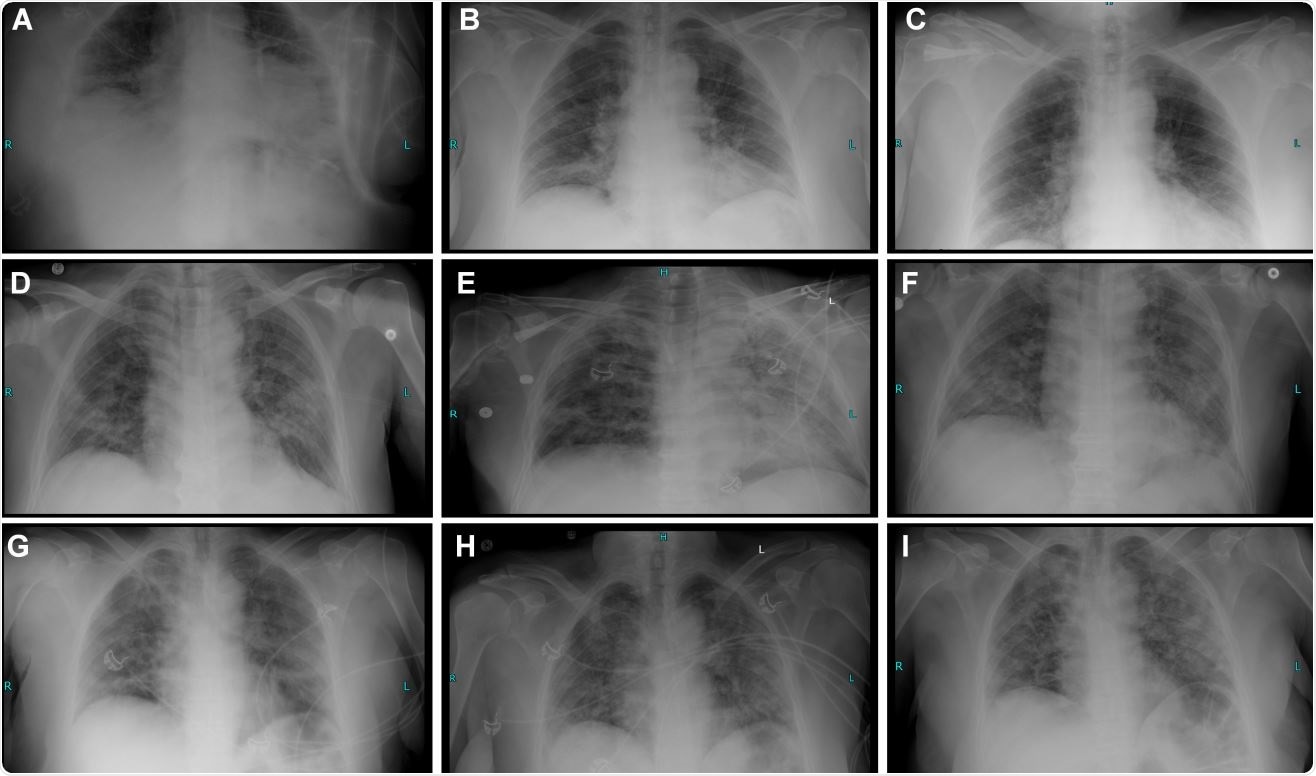
Radiography timeline and clinical course description of 3 COVID-19 cases treated with hemofiltration.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Control of inflammation is a possible therapeutic avenue for COVID-19. The extracorporeal blood purification (EBP) modality is employed to ameliorate maladaptive inflammation.
Rodney Rosalia et al., in a recent medRxiv* preprint research paper, study the longitudinal variation of parameters involved with systemic inflammation in critically ill COVID-19 patients upon EBP treatment. They report that EBP decreases the atypical inflammation - as a means to halt disease progression.
The study cohort was 44 consecutive COVID-19 cases treated with the cycle extracorporeal continuous venovenous hemofiltration (CVVHF) with cytokine adsorbing hemodiafilter (CAH). The AN69ST (oXiris®) cytokine adsorbing hemodiafilter is used here. This device can reduce cytokine levels, support hemodynamic stabilization, and increase survival probability. Here, the researchers perform a time-series analysis of biochemical, inflammatory, blood gas- and vital sign parameters in COVID-19 patients post EBP.
The blood purification is associated with the normalization of several biomarkers that are linked to the COVID19 disease severity. All patients were treated with ≥ 1 cycle CVVHF with CAH.
Of these, 30 severe patients received CVVHF-CAH within 4 – 12 hours of hospitalization. Another 14 patients admitted with mild-to-moderate symptoms progressed to severe disease and placed on EBP during hospitalization.
The suspected hyperinflammation or hypercoagulation correlated with C-reactive protein (CRP), IL-6, Ferritin, or Lactate Dehydrogenase, or D-dimers. IL-6 is the primary inducer of hepatic CRP synthesis and secretion. However, a weaker association between IL-6 and CRP is observed in this study. Ferritin is a biomarker associated with severe COVID-19. Elevated LDH serum concentrations reflect tissue/cell destruction; it is an important biomarker of the severity of idiopathic pulmonary fibrosis.
The treatment progression is associated with a reduction of Ferritin, CRP, Fibrinogen, several inflammatory markers, and a resolution of numerous cytopenias (low cell blood count). The researchers note that cytopenias often accompanied hyperinflammation. EBP has normalized the counts in this study. Hypercoagulability is assessed via Fibrinogen and D-dimers. Consistently, the D-dimers are observed to increase in this study.
It is important to note that oXiris® significantly reduced the CRP levels in non-severe patients but not in severe patients. While hematological parameters showed a continuous decline, the blood urea rose evidently in the severe cohort. The patients who succumbed to COVID-19 showed repetitive measurements of LDH surpassing the critical threshold. The LDH can be a prominent indicator in severe COVID-19 patients to distinguish the need for immediate medical attention.
The researchers, however, note that the clinical severity of COVID-19 does not align with the systemic levels of biomarkers.
Severe patients also experienced a gradual improvement in their low peripheral oxygen saturation (SpO2) and breathing capacity.
The researchers also note a high bacterial co-infections as compared to previous studies. In this study, the mortality was 36.3% across the cohort.
A continued rise in IL-6 is observed in patients who ultimately succumbed to the disease despite repetitive hemofiltration cycles. However, repetitive hemofiltration is associated with lower levels of IL-6 in COVID-19 patients.
In conclusion, the researchers describe in detail the clinical course, outcome, and longitudinal analysis of multiple biomarkers, clinical and blood gas parameters in non-severe vs. severe COVID-19 patients treated with blood purification using the extracorporeal blood purification, with cytokine adsorbing oXiris® hemodiafilter.
This prospective cohort study evaluated the outcome associated with EBP to control hyper inflammation. It shows that EBP improves the condition of patients - associated with an observable reduction of numerous inflammatory mediators, acute phase proteins, and resolution of cytopenias. Thus EBP is an attractive treatment modality to limit systemic damage; therefore, it may be employed to stabilize the clinical condition of severe COVID-19 patients.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Extracorporeal Blood Purification in moderate and severe COVID-19 patients: a prospective cohort study Rodney Rosalia, Petar Ugurov, Dashurie Neziri, Simona Despotovska, Lidija Veljanovska-Kiridjievska, Emilija Kostoska, Dimche Kuzmanov, Aleksandar Trifunovski, Gianluca Villa, Dijana Popevski, Zan Mitrev medRxiv 2020.10.10.20210096; doi: https://doi.org/10.1101/2020.10.10.20210096, https://www.medrxiv.org/content/10.1101/2020.10.10.20210096v1
- Peer reviewed and published scientific report.
Rosalia, Rodney Alexander, Petar Ugurov, Dashurie Neziri, Simona Despotovska, Emilija Kostoska, Lidija Veljanovska-Kiridjievska, Dimche Kuzmanov, et al. 2021. “Extracorporeal Blood Purification in Moderate and Severe COVID-19 Patients: A Prospective Cohort Study.” Blood Purification, June, 1–10. https://doi.org/10.1159/000515627. https://www.karger.com/Article/FullText/515627.