As the world emerged from the shadow of the first wave, most countries relied on testing and case isolation, with contact tracing and quarantine. However, there is a vast difference in the way these strategies are executed from country to country. Some do mass testing of whole populations. Others perform more targeted testing.
While the initial scarcity of tests has largely been overcome, the second wave may see testing capacity being stretched beyond its limits again. Moreover, there is a shortage of information on the disease's clinical profile and its outcomes in those tested vs. those who are positive. Population-based cohort testing is rare among the numerous reports now available.
Wide Differences in Proportion of Positive Tests
The current study aims to identify the characteristics, social, demographic, and clinical, at the time of testing of the patient with COVID-19, and the outcomes after a positive test. This is vital to understand the actual range of severity of the disease and predict the spread of the virus and the future burden it may pose to health services.
The analysis includes over 3.3 million people, of which ~219,000 returned a positive test, between January and June 2020. Patients from three different continents were included.
Comparing the test numbers with the positives found that the proportion of positives among those tested ranged from 2.3:100 to 31.2:100. There was a clear time trend in that the ratio was much higher in February to April (50:100 in April) compared to 6.8:100 in May/June 2020.
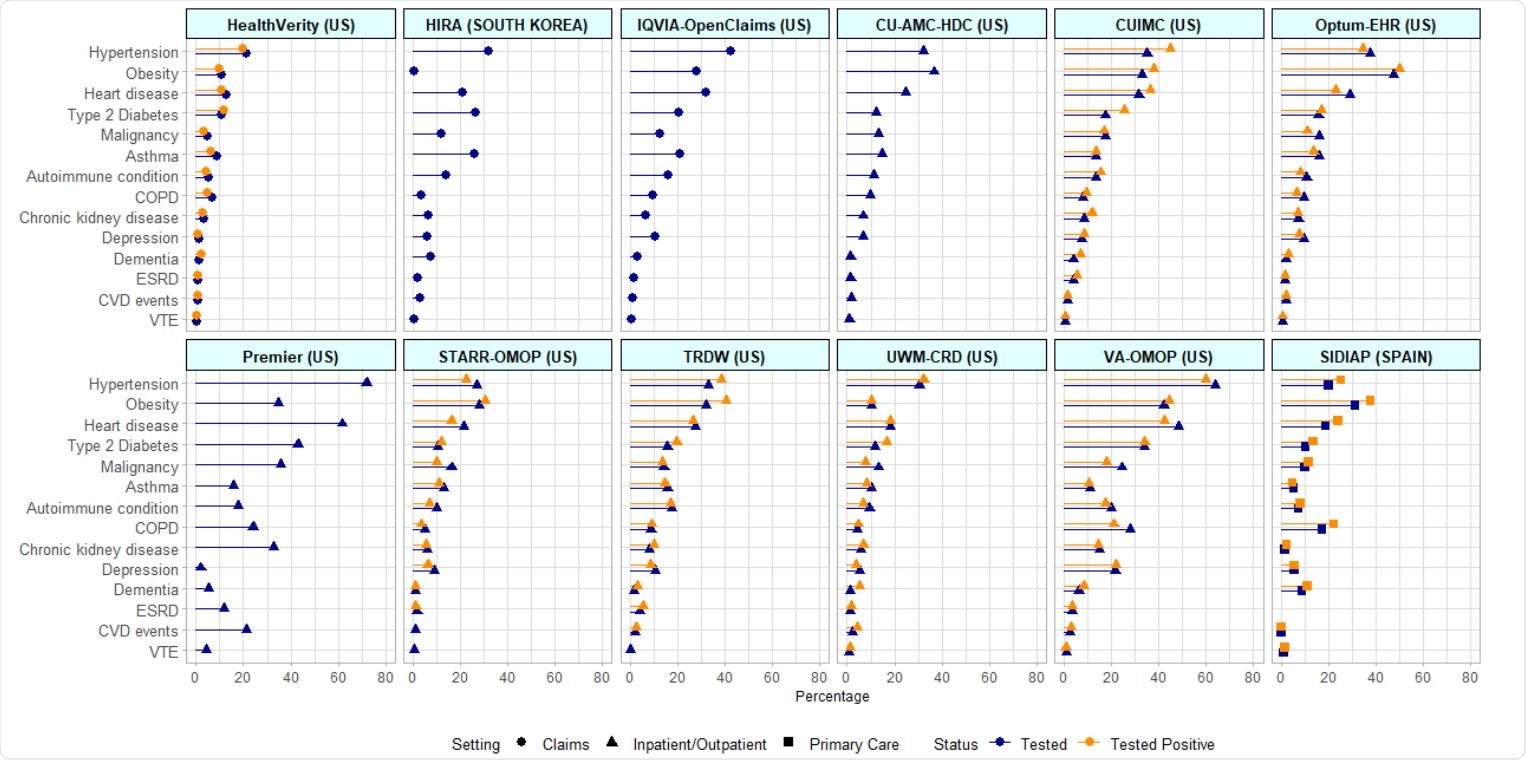
Baseline comorbidities 30-days prior to index date among SARS-CoV-2 tested and tested+ cohorts across databases of various setting

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Sociodemographic factors
Most of the participants were adults below 64 years, with 20% to 48% being over 65, depending on the study. The proportion of women varied from 52% to 64% in almost every study included. The positives usually had a higher prevalence of chronic illness, specifically heart disease and hypertension, at ~42% and ~60% in the positive group vs. 19% and ~20% in the tested group. Obesity was also more common among the positives, at ~44%, versus 31% in the tested group.
Earlier studies have also shown that hypertension, heart disease, and diabetes are more common among those with COVID-19.
Symptoms most commonly reported in the tested group were cough, fever, and shortness of breath. Their prevalence was still higher in the positives, and patients hospitalized for any cause.
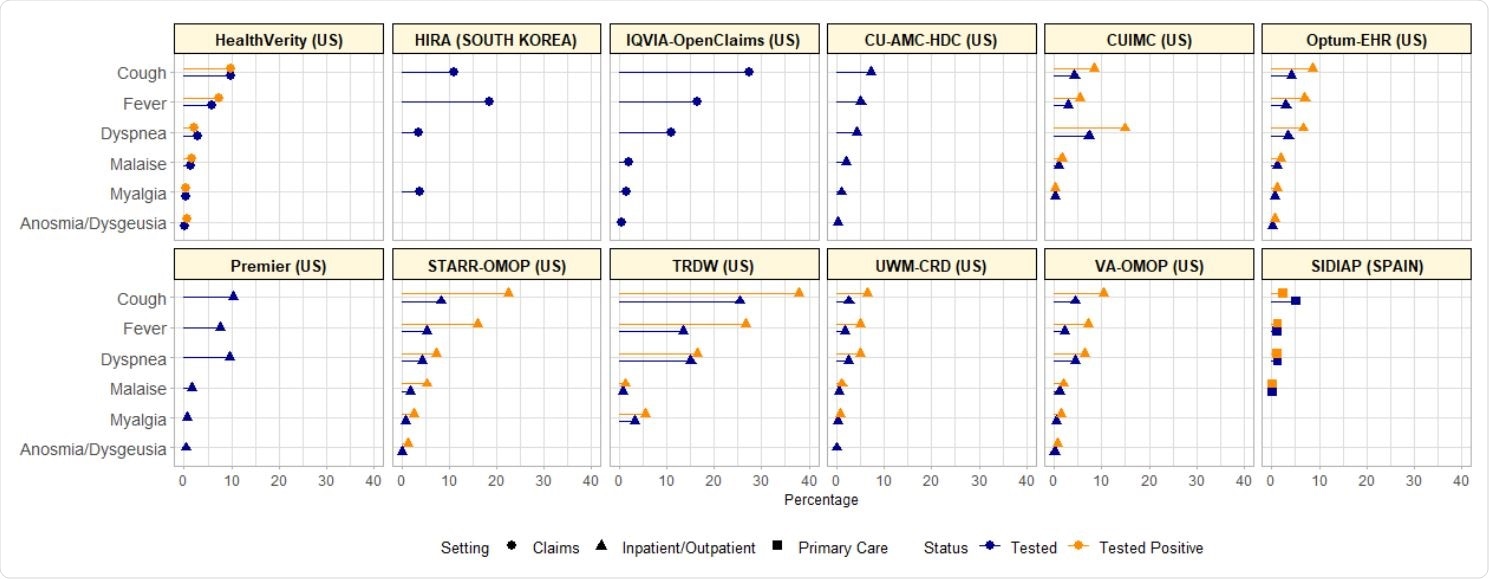
COVID-19 symptoms at index date among SARS-CoV-2 tested and tested+ cohorts across databases of various setting
Outcomes Among Positives
At 30 days from diagnosis, ~4% to ~38% of positives had been hospitalized in various studies. The proportion of deaths in this period ranged from ~9% to ~11%. Outcomes tended to improve over time. The 45% rate of hospitalization in March 2020 declined to ~14% by May, and the 30-day death rate from 11% to ~1% in the same period. Positives with pneumonia in this period made up ~4% to ~22% of the whole, while 1% to 12% developed acute respiratory distress syndrome (ARDS).
Other Complications
Patients who tested positive for COVID-19 had a risk of sepsis ranging from 0.6% to ~5%. In this group, the most frequently occurring kidney complication was acute kidney injury, at up to ~8%, with dialysis being required in 1.5%.
When the total composite cardiovascular event outcome is considered, 0.2% to 5% of these patients were affected. Venous thromboembolism (VTE) was observed in 0.2% to ~2%.
Reasons for Observed Differences
The wide disparity in the proportion of positive results shows the differences in testing strategies and practices and testing coverage. The study also brought out a significant change in testing with time up to May/June 2020.
Though it is now beyond doubt that COVID-19 disproportionately affects the elderly and the male sex, the majority of those tested and of the positives were females and below 64 years. The reasons attributed to this phenomenon include increased exposure for females in the workplace, such as in hospitals or nursing homes, or the fact that women may seek testing more often.
Chronic illnesses are more common among the positives, perhaps because they are more likely to be tested because of these diseases or because they, or the treatment of these conditions, promote SARS-CoV-2 infection.
Severe and Critical Disease
The analysis shows an overall range of severe disease requiring hospitalization in 4% to 38% of the positives. These patients were also more likely to develop ARDS and several other systemic complications. This agrees with other reports, such as those from the US Centers for Disease Control and Prevention (CDC).
However, as more cases are diagnosed with less severe disease, the proportion of hospitalized cases will probably go down. The high mortality of 4% to 11% within a month of the first positive test is perhaps because the figures come from the peak pandemic months.
Implications
This is the largest group of patients to have COVID-19 tests, test reports, and baseline characteristics reported. The investigators used 12 databases from across three continents.
The authors conclude, “Our study suggests that symptoms such as cough and fever remain key disease features, predictive of a positive test.” However, these are somewhat nonspecific symptoms, and their value in discriminating between COVID-19 and other conditions like influenza needs to be carefully examined in future studies.
An important fringe benefit was that an indirect assessment of the population with a negative COVID-19 test could be carried out, comprising ~93% of the whole tested cohort. Therefore, they are responsible for the differences in patient characteristics and outcomes between the tested and positives.
The challenge facing public health authorities is to ensure adequate testing capacity for the second wave, keeping the proportion of positives low, at below 5%, to ensure the pandemic remains under control.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.