The study showed that by July, with the exception of unstable angina and acute alcohol-related events, the primary care contact rates across all the acute physical and mental health conditions studied had not returned to pre-lockdown levels.
The team’s analysis of electronic health records from general practices showed the most dramatic drops in primary care contacts were for diabetic emergencies, depression and self-harm.
“Our study is the first to explore the effect of lockdown measures on primary care contacts for specific acute physical and mental health conditions across the UK,” says Kathryn Mansfield (LSHTM) and colleagues.
The team says it is likely that much of the deficit in care observed here represents a considerable burden of unmet need, with implications for subsequent morbidity and premature mortality.
The conditions the team studied are sufficiently severe that such unmet needs will have significant ramifications for patients.
The researchers say access to healthcare must be prioritized in the future as part of maintaining public health planning, including after the implementation of further restrictions.
“Health service providers should take steps to prepare for increased demand in the coming months and years due to the short and long-term ramifications of reduced access to care for severe acute physical and mental health conditions,” they write.
A pre-print version of the paper is available in the server medRxiv* while the article undergoes peer review.
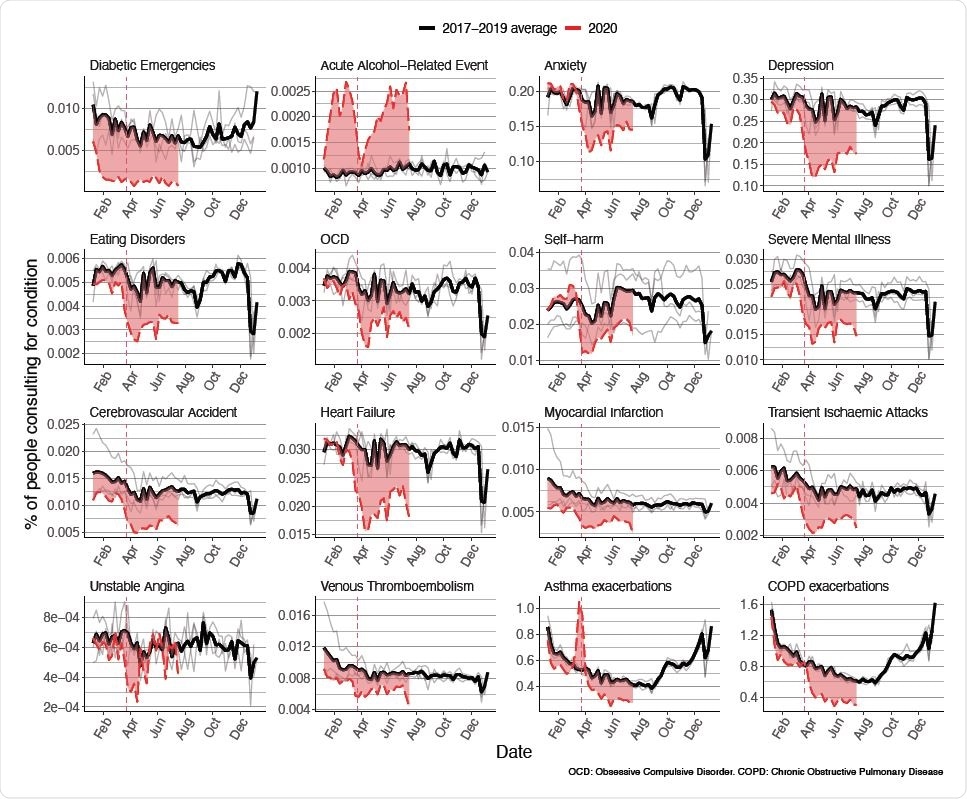
Percentage of study populations with contacts for all conditions in 2017-2019 and 2020. Percentage of eligible population with contacts for each health condition studied in 2020 compared to historical average for that week. Black line, weekly historical average percentage of eligible population consulting (2017-2019, grey lines show the data for 2017, 2018, and 2019). Red dashed line, weekly percentage of eligible percentage consulting in 2020. Red region shows difference with historical average. Red dotted line, introduction of restrictions in UK on March 23rd

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Concerns about physical and mental health since lockdown
Since the UK Government first introduced lockdown measures on March 23rd, 2020, concerns have grown that the response to the pandemic may have negatively impacted physical and mental health and reduced the use of primary care health services.
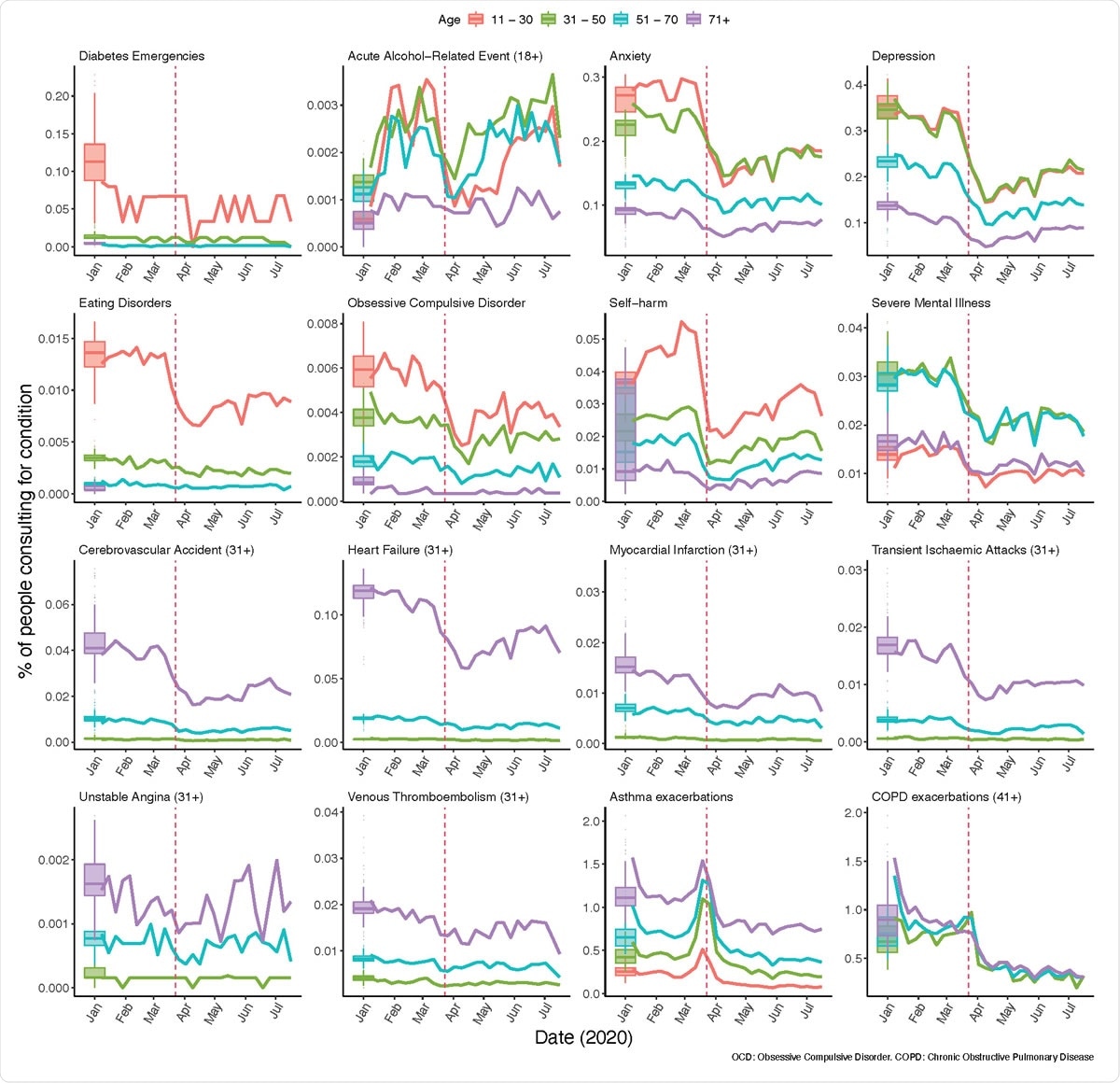
Percentage of the study populations with contacts by age group. Percentage of the study populations with GP contacts for study conditions over 2020, by age group. Boxplots, historical average percentage of study population with GP contacts for the condition of interest. Colored lines, weekly percentage of the eligible population with primary care contacts for the condition of interest in 2020. Red dotted line, introduction of restrictions in UK on March 23rd. Note that cell counts with fewer than five contacts in one week in 2020 have been suppressed.
Reports have indicated that non-COVID-19 related hospital admissions and attendance to A&E departments have declined in the country since March, particularly for myocardial infarctions and cerebrovascular accidents.
However, it is not yet clear what has happened in primary care, where clinical practice has quickly shifted to including more remote consultations.
“There is no published evidence specifically investigating the changes in primary care contacts for severe acute physical and mental health conditions,” said Mansfield and team.
“Understanding the indirect effects of the pandemic and its control measures is essential for public health planning, particularly when/if the COVID-19 pandemic is under control (or if further restrictions are needed), and for informing control measures for future pandemics.”
Analyzing primary care health data for nearly 10 million people
The researchers assessed routinely collected primary care electronic health records from general practices, covering almost 10 million individuals across the UK.
They calculated weekly primary care contacts (including face-to-face or remote consultations and details of diagnoses from hospital discharge notes) for mental health, acute alcohol-related events, exacerbations of asthma/chronic obstructive pulmonary disease (COPD), and cardiovascular and diabetic emergencies.
They compared data available for the three years prior to the pandemic (from January 1st, 2017) with data recorded between the introduction of lockdown on March 23rd and July 12th, 2020.
Primary care contacts fell dramatically across all conditions studied
The total study population included 9,863,903 individuals on January 1st, 2017.
For all conditions studied, primary care contacts dropped substantially following the introduction of lockdown.
With the exception of unstable angina and acute alcohol-related events, the rate of primary care contacts had not returned to pre-lockdown levels by July.
The largest reductions in primary care contacts were observed for diabetic emergencies, depression and self-harm.
Among the general population, estimates of the absolute reduction in primary care contacts up to July, compared with what would have been expected during previous years, varied from fewer than 10 contacts per million for some cardiovascular outcomes, to as many as 12,800 per million for depression and 6,600 per million for anxiety. For COPD exacerbations, the estimated reduction was 43,900 per million.
“Maintaining access to primary care is key”
The researchers say the findings likely represent a large burden of unmet need, particularly in relation to COPD and mental health conditions.
Health service providers should take steps to prepare for increases in morbidity and mortality due to the reduced access to care for severe acute physical and mental health conditions, say Mansfield and team.
“Further research should address whether reduced clinical contact has resulted in excess mortality, and whether we need to increase service provision for individuals with increased healthcare needs resulting from delaying seeking access to care,” they add.
“Maintaining access to primary care is key to future public health planning in relation to the pandemic,” the researchers warn.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Mansfield K, et al. COVID-19 collateral: Indirect acute effects of the pandemic on physical and mental health in the UK. medRxiv, 2020. doi: https://doi.org/10.1101/2020.10.29.20222174, https://www.medrxiv.org/content/10.1101/2020.10.29.20222174v1
- Peer reviewed and published scientific report.
Mansfield, Kathryn E, Rohini Mathur, John Tazare, Alasdair D Henderson, Amy R Mulick, Helena Carreira, Anthony A Matthews, et al. 2021. “Indirect Acute Effects of the COVID-19 Pandemic on Physical and Mental Health in the UK: A Population-Based Study.” The Lancet Digital Health 3 (4). https://doi.org/10.1016/s2589-7500(21)00017-0. https://www.thelancet.com/journals/landig/article/PIIS2589-7500(21)00017-0/fulltext.