A single-center study from Wuhan in China presents ultrasound imaging evidence supporting the notion that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can cause infection of the testis or epididymis – and put patients at risk for further complications. The paper can be found in the Journal of Ultrasound in Medicine.
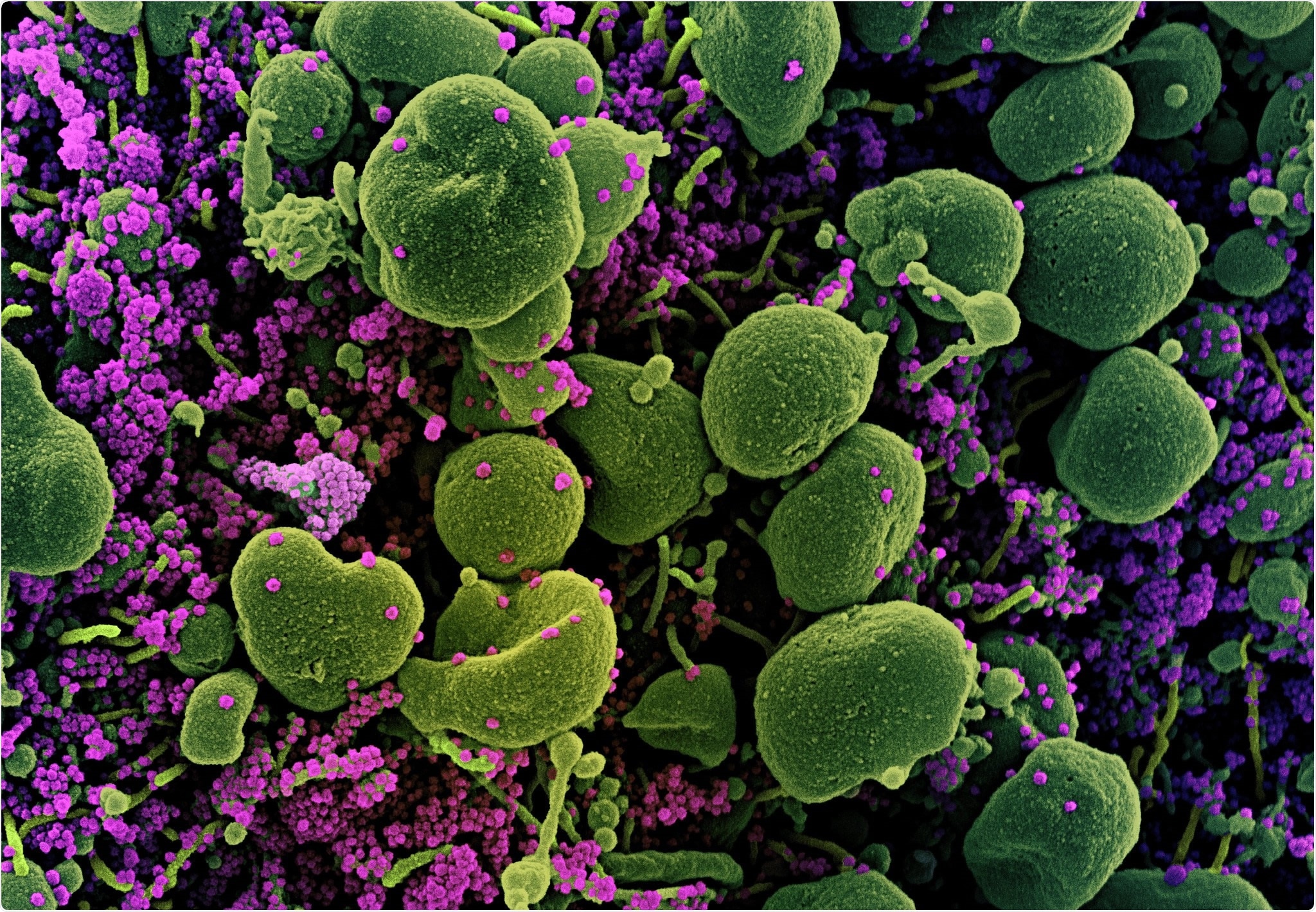
Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-CoV-2 virus particles (purple), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Previous studies have already shown that SARS-CoV-2, a causative agent of coronavirus disease (COVID-19), enters a host cell by utilizing its receptor‐binding domain (RBD) that recognizes a specific cell surface receptor. In humans, angiotensin‐converting enzyme 2 (ACE2) has been pinpointed as the major functional receptor for the RBD of SARS‐CoV and SARS‐CoV‐2.
The expression pattern of ACE2 implies that SARS‐CoV‐2 could affect the function of multiple organs in the human body. More specifically, some previous and recent studies on coronaviruses have demonstrated that this virus can indeed affect many organs beyond the lungs, such as the kidneys, digestive tract, brain, liver, heart, thyroid gland, and testicles.
When human testis tissue is concerned, ACE2 is essentially expressed in undifferentiated male germ cells (spermatogonia), Setoli cells, and Leydig cells. Hence, if we assume receptor interaction regarding the distribution of ACE2, there are reasons to believe that SARS‐CoV‐2 can attack both the testis and the epididymis.
In a recent study, a research group from China (led by Dr. Liao Chen from the Department of Ultrasound Imaging at the Wuhan University Renmin Hospital) acquired direct ultrasound imaging findings of acute scrotal infection in patients hospitalized with COVID‐19 during the pandemic.
A retrospective study of hospitalized COVID-19 patients
This retrospective study included male patients with a confirmed diagnosis of COVID‐19 during their hospitalization in the early days of the pandemic, which also had a bedside ultrasound examination of the scrotum with a delay of 1 week to 1 month after the initial symptoms of the disease.
The scrotal ultrasound examinations concentrated on the imaging manifestations related to the acute orchitis, epididymitis, and epididymo-orchitis, with the subsequent use of specific diagnostic criteria. Furthermore, the proportion of observed epididymo-orchitis was compared in patients belonging to different age and COVID‐19 severity groups.
The ultrasound images for every case were read by two ultrasound specialists; in instances when their impressions were in disagreement, the final verdict was made by a senior professor specialized in imaging diagnosis of male urogenital/reproductive system diseases and with more than twenty years of professional experience.
Major ultrasound imaging findings
From a total of 142 patients with COVID‐19 enrolled in this study, 39 of them (27.5%) showed inflammatory imaging hallmarks such as a thickened fibrous covering of the testis (tunica albuginea), increased blood flow in blood vessels tissue enlargement, scrotal swelling due to hydrocele or abscesses.
Moreover, a total of 32 patients (22.5%) had a diagnosis of acute inflammation of one or both testicles, epididymitis, or both (epididymo‐orchitis) in accordance with the diagnostic criteria. The observed risk of acute scrotal infection also increased with age, reaching 53.3% in patients that were older than 80 years of age.
The researchers have also observed that men presenting with severe COVID‐19 had a substantially higher possibility of developing epididymo-orchitis in comparison to the COVID‐19 group without severe disease. All of this means that the testicles are indeed a potential target of SARS-CoV-2.
Nonetheless, it must be noted that many patients with COVID‐19 are in a state of diminished immunity, which enables bacteria from the ascending urinary tract to break out and cause scrotal infections. In addition, hormonal dysregulation is also present and may compound this problem.
Implications for clinical practice
In a nutshell, this study's results support the notion that SARS‐CoV‐2 infection may specifically affect the testis, epididymis, or both. Of course, systemic inflammatory reaction and present co-morbidities have to be taken into account because they can also result in tissue enlargement and testicular swelling.
"We suggest that clinicians remain aware of the risk of acute scrotal infection in hospitalized patients with COVID‐19, and for young male patients with COVID‐19 (especially those who wish to have children) local symptoms and fertility should be carefully monitored and protected", caution study authors.
In any case, further research endeavors based on biopsy or autopsy should be conducted to ascertain whether pathologic and histologic changes caused by SARS‐CoV‐2 can be found in the testis and epididymis of patients with COVID‐19.