A recent systematic review and meta-analysis conducted by a team of international scientists reveal low seroprevalence of anti-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibodies in the general population.
According to the study’s findings, estimating seroprevalence may be a better approach to complement SARS-CoV-2 infection testing and to ascertain a more accurate picture of the global burden of the pandemic. The study is currently available on the medRxiv* preprint server.
Since its emergence in December 2019, the highly infectious SARS-CoV-2, the causative pathogen of coronavirus disease 2019 (COVID-19), has infected more than 56.5 million people and claimed more than 1.35 million lives worldwide. Although several measures have been taken to improve the quality and quantity of testing, the exact global prevalence of SARS-CoV-2 infection seems to be higher than the reported prevalence because of limited availability and accessibility of testing in socioeconomically deprived countries. Moreover, an increased prevalence of asymptomatic cases could be another significant reason for such underestimated COVID-19 incidence.
Diagnosis of COVID-19 is most commonly done by rapid antigen testing or polymerase chain reaction (PCR)-based viral RNA testing using nasopharyngeal swabs or saliva samples. In contrast, an antibody assay is generally performed to determine the presence of anti-SARS-CoV-2 antibodies in blood samples. A positive antibody test indicates past SARS-CoV-2 infection in non-vaccinated people. Hence, serological antibody testing provides a more accurate estimation of previous infections in the general population.
Many studies have been done nationally as well as regionally to estimate the seroprevalence of SARS-CoV-2 antibodies in the general population. These seroepidemiological studies are particularly important for identifying high-risk groups. Population-based seroepidemiological data can be used as a reference to optimally strategize public health measures and the distribution of COVID-19 vaccines.
Current study design
The scientists systematically reviewed and analyzed many seroepidemiological study findings to more accurately estimate the global prevalence of SARS-CoV-2 infection. Their search included peer-reviewed articles, preprint articles, and other non-commercial/non-academic articles that were published between January 1 and August 28, 2020. They used various statistical analytical methods to identify demographic differences in seroprevalence and study-level factors associated with seroprevalence. To better estimate the global seroprevalence, they corrected available study findings for test sensitivity and specificity.
Important observations
A total of 338 seroepidemiological studies were analyzed. These studies involved 2.3 million individuals from 50 countries. About 54% and 46% of the studies were conducted in the general population and special populations (specific occupation, health status, and COVID-19 exposure status), respectively.
The current study analysis revealed that the SARS-CoV-2 antibody seroprevalence was as low as 3.2% in the general population. Similarly, the seroprevalence was 5.4% in at-risk populations (special populations). Regarding frontline workers, the presence of anti-SARS-CoV-2 antibodies were detected in 6.3% and 10% of healthcare workers and essential non-healthcare workers, respectively. Compared to the general population, healthcare workers were 1.7 times more likely to be seropositive. Similarly, people with established contact exposure were also susceptible to develop anti-SARS-CoV-2 antibodies.
A comparatively lower seroprevalence was observed in high-income countries (3.4%). However, differences in estimated seroprevalence were observed in low- and middle-income WHO Global Burden of Disease (GBD) regions, ranging from 1.0% in Southeast Asia, East Asia, and Oceania to 18.8% in South Asia. Despite having a higher risk of SARS-CoV-2 transmission and poor COVID-19 prognosis, the number of studies conducted in low- and middle-income countries was low (25%).
Regarding demographic characteristics, a higher seroprevalence is observed in people ages 18 to 64 years compared to those ages 65 years and above. White people were less likely to have anti-SARS-CoV-2 antibodies than black people and Asian people.
Most importantly, the scientists observed that the seroprevalence estimates were 14.5 times higher than the corresponding collective prevalence of COVID-19 cases. This difference became more noticeable when local seroprevalence studies were included for analysis. Relatively higher frequencies of local studies conducted in COVID-19 hotspots may be the reason for such discrepancy.
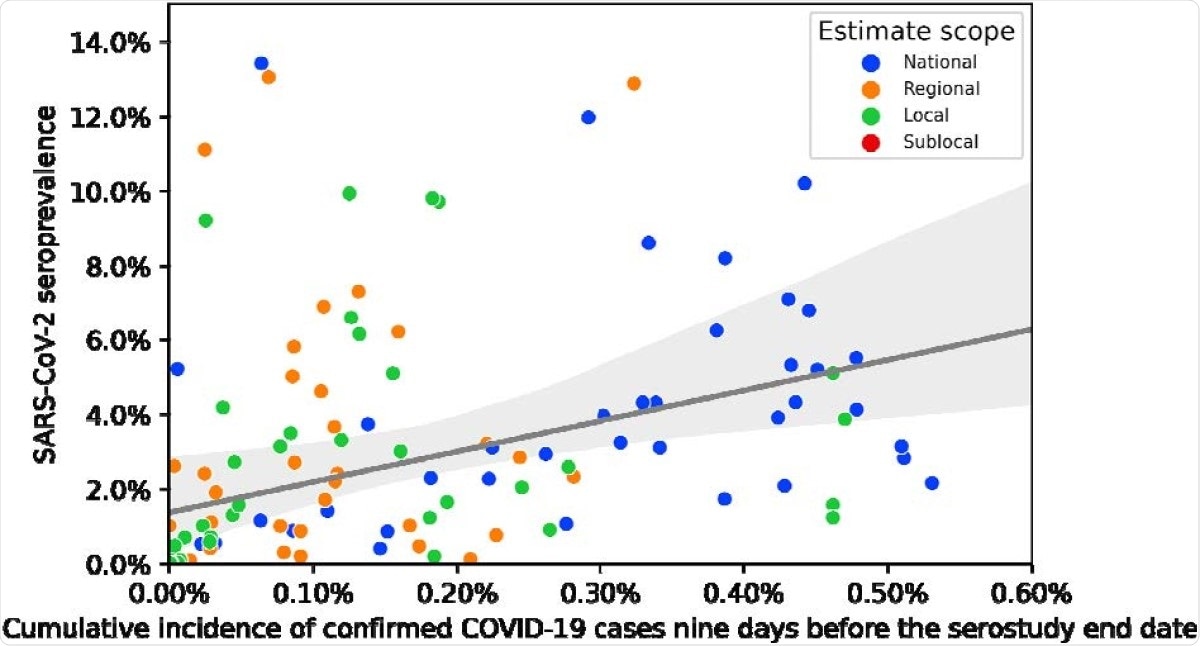
Seroprevalence to cumulative case incidence ratios using cumulative incidence nine days prior to the serosurvey end date.
Overall, these findings indicate that estimating only confirmed COVID-19 cases is not sufficient to determine the actual burden of SARS-CoV-2 infection. By analyzing seroprevalence to collective COVID-19 incidence ratios, the scientists indicate that about 643 million people may have already been infected by SARS-CoV-2 globally, which is much more than the reported COVID-19 cases (currently 56.5 million).