Researchers in China have conducted a study suggesting that people who have recovered from coronavirus disease 2019 (COVID-19) may not pose a risk to close contacts if they become reinfected with the causative agent severe acute respiratory syndrome coronavirus (SARS-CoV-2).
The study found that more than a thousand people in Wuhan who tested positive for reinfection with SARS-CoV-2 after having recovered from COVID-19 and being discharged from hospital, did not cause new infections among any of the people who lived in the same house as them.
Among 1,265 recovered patients who tested positive for SARS-CoV-2 again (repeat positive) after returning home from hospital, none of their 4,079 close contacts tested positive for the virus.
“This indicates that patients with repeat positive don’t cause new infections,” say Huaiyu Tian from Beijing Normal University and colleagues.
A pre-print version of the paper is available on the medRxiv* server while the article undergoes peer review.
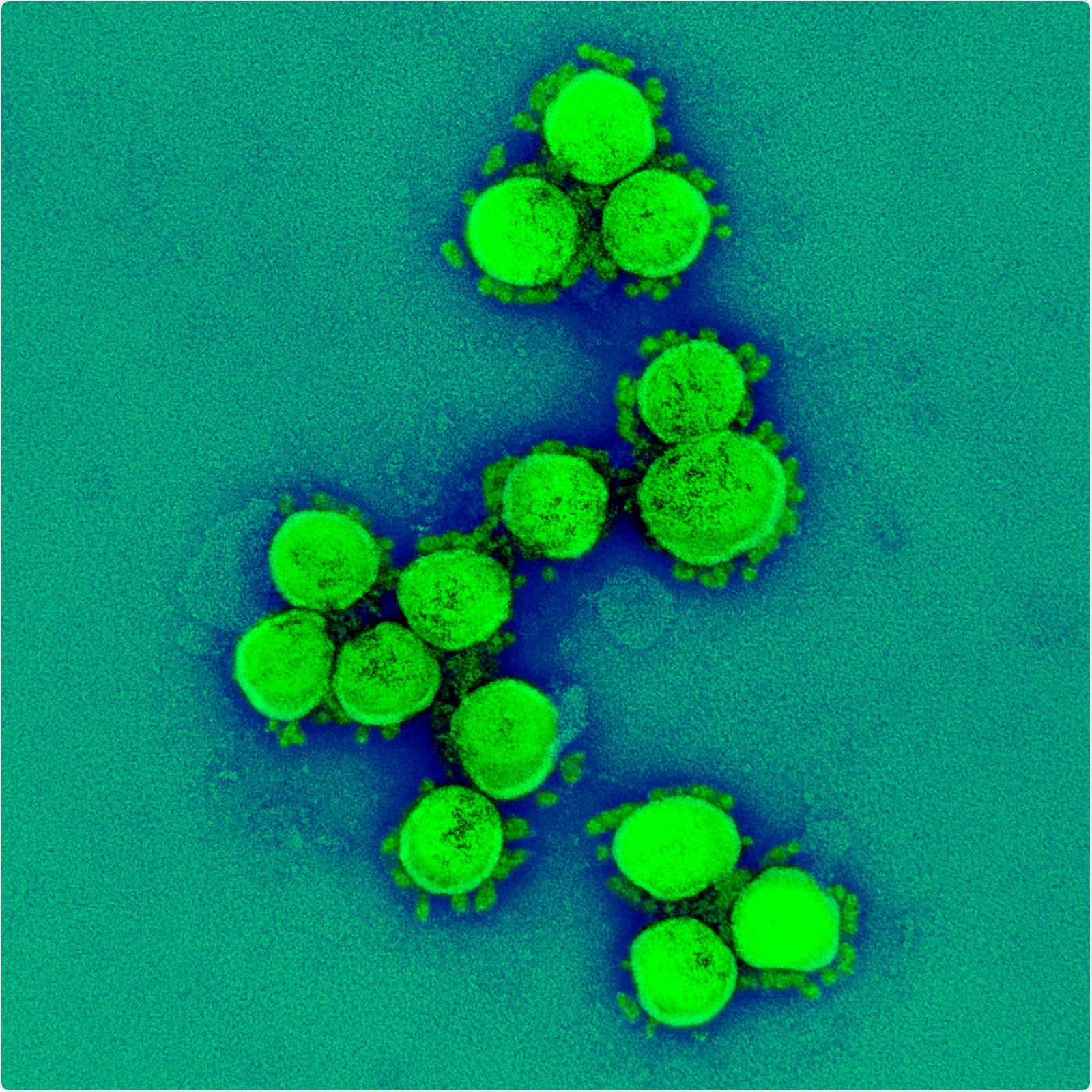
Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
What are the current recommendations?
Guidelines from the World Health Organization (WHO) recommend that a patient who has recovered from COVID-19 should test negative for SARS-CoV-2 twice (with a sample interval of at least 24 hours) before they are discharged from hospital.
In Wuhan, patients then self-isolate for 14 days in a rehabilitation center and for a further 14 days at home. Patients are required to return to hospital for follow-up visits at two and four weeks following discharge.
Reports have suggested that some convalescent patients test repeat positive during the isolation periods, although most of these reports have been based on limited sample size, say Tian and the team.
“Understanding the epidemiological characteristics of patients with repeat positive is vital in preventing a second wave of COVID-19,” they write.
What did the researchers do?
The researchers retrospectively analyzed clinical and epidemiologic data available for a cohort of 20,280 COVID-19 patients from 84 hospitals in Wuhan between 31st December 2019 and 4th August 2020.
Nasopharyngeal swabs or pharynx swabs were collected and tested for SARS-CoV-2. Repeat positives were confirmed by reverse transcriptase-polymerase chain reaction (RT-PCR).
To investigate whether patients who were repeat positive may cause new cases of infection, the researchers also tested individuals who shared households with them.
What did the study find?
Of the 20,280 recovered patients, 2,466 (12.16%) tested repeat positive for SARS-CoV-2 following hospital discharge.
The median time a patient was hospitalized for (treatment time) during the first infection was significantly longer among patients who tested repeat positive than among those who did not, at 18.5 versus 15.7 days.
Among patients who tested repeat positive, the median treatment time for the second infection was shorter (10.6 days) than for the first infection (18.5 days).
The median time interval between hospital discharge and the identification of a repeat infection was 11 days.
Logistic regression analysis revealed that age was not associated with the risk of testing repeat positive.
Interestingly, the team found that gender played a role, with males at a significantly lower risk of developing a repeat infection than females.
Of 2,466 patients who were repeat positive, 1,201 tested positive in a rehabilitation center, where no individuals had close contact with them.
“So these 1,201 patients had no chance to infect healthy persons,” writes the team.
The remaining 1,265 patients tested positive once they were back at home, and, between them, they had shared households with 4,079 individuals.
However, the RT-PCR results for these close contacts showed that none of them were positive for SARS-CoV-2.
What did the authors conclude?
Although many patients became reinfected, the researchers say that most appear to have not caused any new infections following their discharge from hospital.
“In this follow-up study in Wuhan, we show the basic characteristics of patients with repeat positive and no new infections caused by patients with repeat positive of COVID-19,” they write.
The team says a study conducted earlier this year found that no infectious SARS-CoV-2 could be obtained, and no full-length genomes could be sequenced from samples that had been taken from 87 cases of repeat positives.
“This may explain why there were no secondary infections,” suggest Tian and colleagues.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Tian H, et al. A follow-up study shows no new infections caused by patients with repeat positive of COVID-19 in Wuhan. medRxiv, 2020. doi: https://doi.org/10.1101/2020.11.18.20232892, https://www.medrxiv.org/content/10.1101/2020.11.18.20232892v1
- Peer reviewed and published scientific report.
Wu, Xiaomin, Zengmiao Wang, Zhenyu He, Yapin Li, Yating Wu, Huaiji Wang, Yonghong Liu, Fanghua Hao, and Huaiyu Tian. 2021. “A Follow-up Study Shows That Recovered Patients with Re-Positive PCR Test in Wuhan May Not Be Infectious.” BMC Medicine 19 (1). https://doi.org/10.1186/s12916-021-01954-1. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-01954-1.