Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the causative pathogen of coronavirus disease 2019 (COVID-19) – continues to spread worldwide. 58.8 million people have been infected with the virus across 191 countries and territories, and 1.41 million have lost their lives.
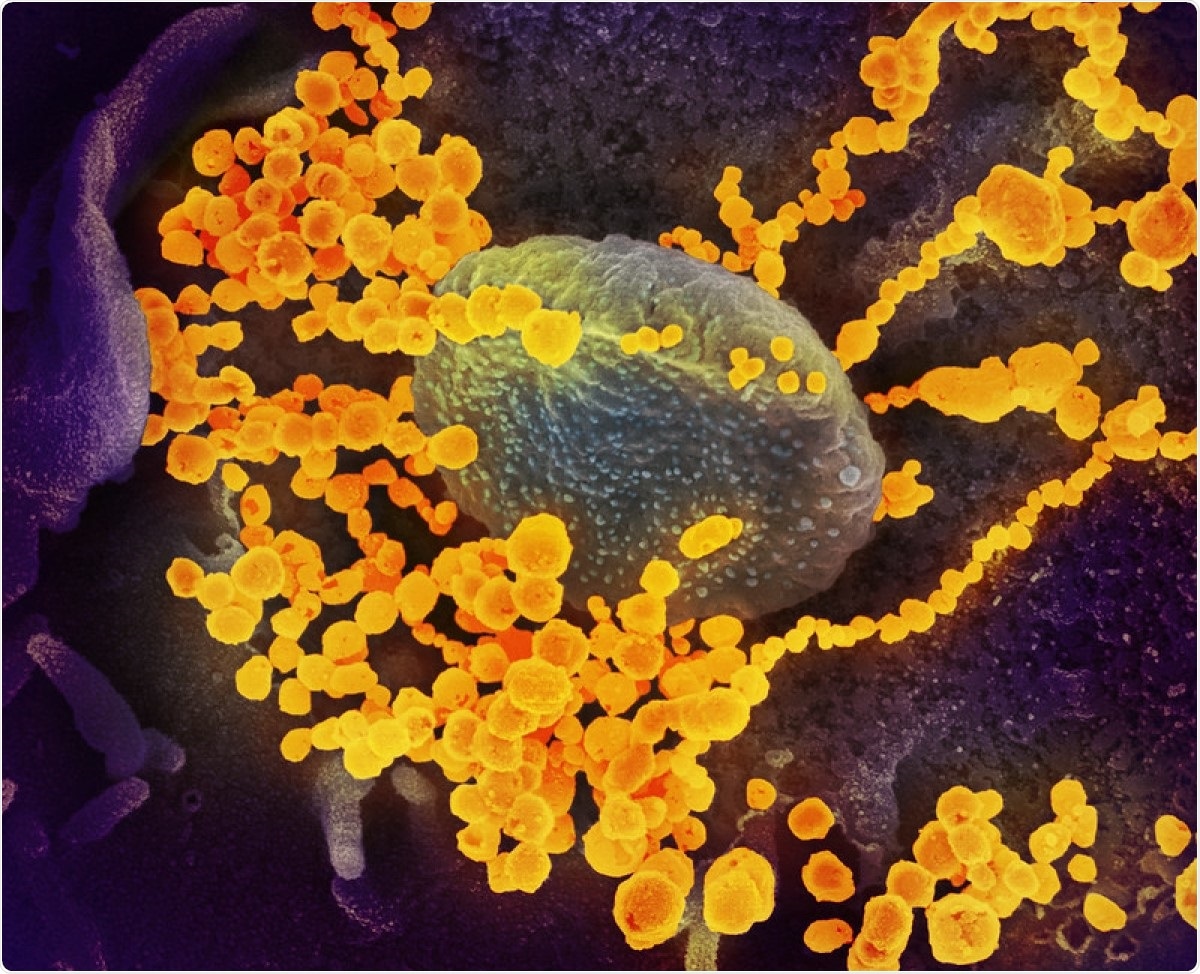
This scanning electron microscope image shows SARS-CoV-2 (round gold objects) emerging from the surface of cells cultured in the lab. SARS-CoV-2, also known as 2019-nCoV, is the virus that causes COVID-19. The virus shown was isolated from a patient in the U.S. Image captured and colorized at NIAID's Rocky Mountain Laboratories (RML) in Hamilton, Montana. Image Credit: NIAID / Flickr
The development of safe and effective vaccines that can immunize against SARS-CoV-2 is still ongoing. A number of promising vaccine candidates have now entered their final phase of clinical trials or are awaiting regulatory body approval.
However, it will likely be some time before any of the vaccine candidates are fully approved and ready for widescale administration to the global population; a mammoth task that national and global public health authorities all over the world are now grappling with the complex logistics of.
As the prospect of widescale vaccination remains somewhat distant, and COVID-19 cases continue to climb worldwide, many researchers continue the hunt for effective therapeutics that can mitigate the impact of SARS-CoV-2 infection on those severely or critically ill. Such measures are crucial in aiding patient recovery and preventing mortality in those with more serious COVID-19 cases and underlying conditions or comorbidities that increase their chance of death.
A recent study based at a hospital in Buenos Aires, Argentina, found that convalescent plasma therapy for patients with severe COVID-19, and COVID-19-related pneumonia, was largely ineffective. These findings, if corroborated by further study in the area, may well mean that we need to look elsewhere for effective antiviral treatment while vaccines are still on the way.
The researchers have published their findings in the latest issue of the New England Journal of Medicine.
What is convalescent plasma?
Convalescent plasma therapy for COVID-19 is a form of clinical treatment where blood plasma containing anti-SARS-CoV-2 antibodies is taken from recovered patients and administered to those with severe or critical disease.
As a therapeutic method, convalescent plasma has been used for centuries to combat many pathogens, note the researchers, and is believed to be an effective way of promoting ‘passive immunity’ in an infected patient.
It is typically thought “that passive immunization can ‘jump start’ the immune system to control the evolution of the disease until a specific immune response is established in the infected person,” they write.
The study
In total, 333 patients were enrolled in the test; 228 patients received convalescent plasma, while 105, as a control group, received a placebo.
From symptom onset to trial enrolment, the median time was 8 days, and hypoxemia (abnormally low oxygen levels in the blood) was the most common severity criterion for enrollment.
The infused convalescent plasma that the first group was administered had a median titer of 1:3200 of total SARS-CoV-2 antibodies.
The primary measure of outcome was the patients’ clinical status and condition 30 days after the intervention, as measured along a six-time-point scale with an ordinal scale ranging from total recovery to mortality.
The study’s findings
Overall, the researchers found a negligible difference in the convalescent plasma group and the control group.
“At day 30, no significant difference was noted between the convalescent plasma group and the placebo group in the distribution of clinical outcomes according to the ordinal scale (odds ratio, 0.83 (95% confidence interval [CI], 0.52 to 1.35; P = 0.46).”
Mortality was 10.96% in the convalescent plasma group and 11.43% in the placebo group, for a risk difference of around 0.46 percent.
Despite previous studies that have touted the putative benefits of this common antiviral method – for COVID-19 and other coronavirus and non-coronavirus infections, including SARS, MERS, and influenza – the researchers believe that their randomized data-pool has shown a much lower, but more accurate, efficacy rate than has previously been thought.
For them, this finding “illustrates the importance of randomized, controlled trials, especially in the context of a pandemic.”
These findings are perhaps a sober reminder that safe, effective and targeted therapies for COVID-19 are yet to be developed. The discovery or development of efficacious antivirals and other therapeutic methods remains urgent, while widescale vaccination or herd immunity remains a distant prospect.
Source:
Journal reference: