The coronavirus disease 2019 (COVID-19) pandemic has taken a toll on many countries, especially those with a skyrocketing number of cases. COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has emerged as a worldwide pandemic, infecting over 69 million people.
The virus can attack and infect anyone, regardless of social status. But a new study by researchers at the St Michael's Hospital, Canada, and Harvard University, USA, have found that people in less privileged neighborhoods are at a higher risk of being infected with SARS-CoV-2 and of more severe COVID-19.
Like many other health outcomes, the impact of COVID-19 has been marked by racial, ethnic, and class inequalities. For instance, the U.S. Centers for Disease Control and Prevention (CDC) reports that racial disparities in COVID-19 have led to disproportionate hospitalizations and deaths.
The health agency added that non-Hispanic Black, African American, Hispanic or Latino, and American Indian or Alaska Native individuals are around three times more likely to have been diagnosed with COVID-19. Also, they are five times more likely to be hospitalized, and up to two times more likely to die compared to White people.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
The study
The study, published in the pre-print journal medRxiv*, evaluated neighborhood-level inequities in terms of income, racism, racialized economic segregation, and racialized occupational segregation.
The researchers visited health department websites for the 69 urban counties in the United States to determine counties for which data were available. The primary outcome of interest in the study was the rate of cumulative COVID-19 cases in each neighborhood, and the secondary results include the rates of cumulative deaths, tests, and test positivity.
What the study found
The study's findings showed that, out of the 69 urban counties in the US, 58 had case data available at smaller geographic units. There was a total of 85 million population, with 1.8 million cumulative cases. This represented over a quarter of all reported cases in the US and Canada during the data collection.
Further, the team reported inequities across a large number of cities. They compiled a dataset of neighborhood-level outcomes. They presented city-specific rates and trends, including considerable variations within cities. For instance, they found that urban regions with the highest and second-highest infections were 2,800 per 100,000. However, in the most privileged area and the most deprived area, the difference was 730 per 100,000.
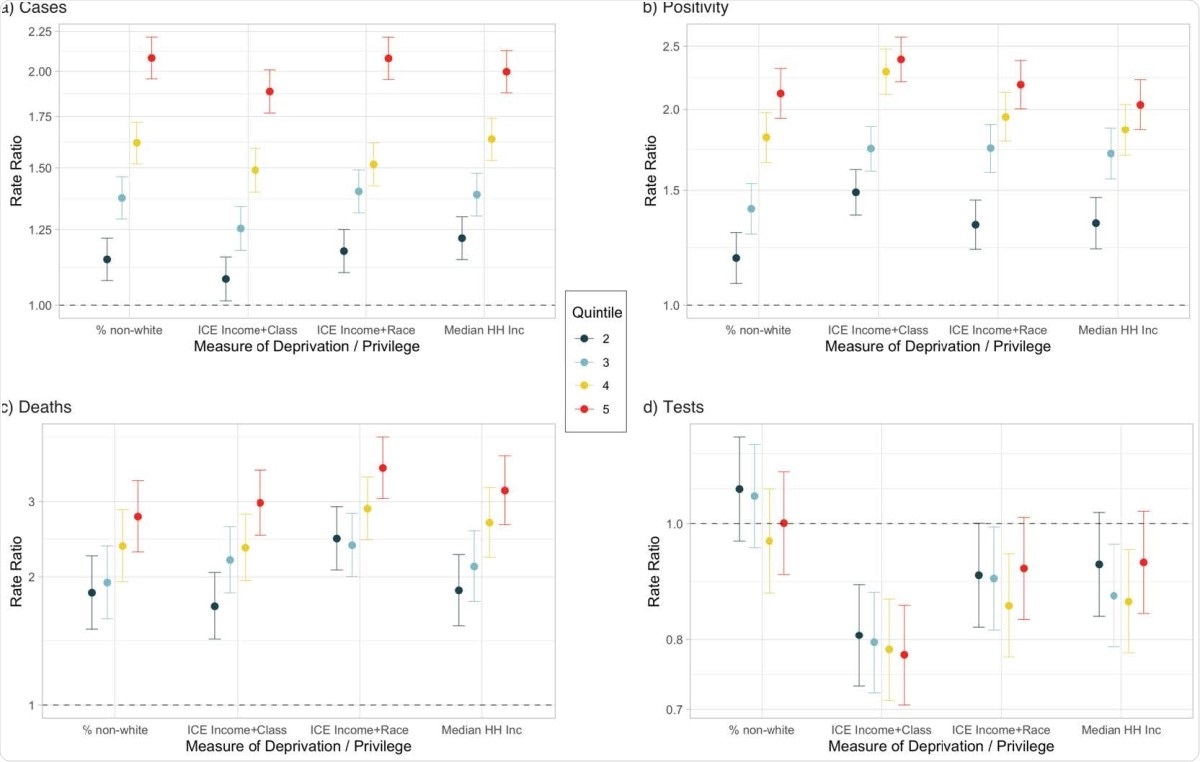
Rate ratios for COVID-19 a) cases, b) positivity, c) deaths, and d) tests from multilevel Poisson models for quintiles of Median Household Income, Percentage of non-white population, Index of Concentration at the Extremes for Race and Income, and Race and Working Class. The most privileged quintile is the referent category for each measure.
In a nutshell, the team found persistent evidence of social gradients for the case, death, and positivity rates. The most privileged neighborhoods have lower rates, but no variation in the magnitude of inequities between cities.
However, the team also noted that gradients were not apparent testing rates, which means inadequate testing in the most deprived neighborhoods.
With the study findings, the team suggests that health agencies monitor inequities as part of the COVID-19 reporting to guide response efforts in controlling and containing the virus spread.
The US currently has the highest number of cases worldwide, topping 15.39 million. Of these, more than 289,000 have died due to COVID-19.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Source:
Journal reference: