An interesting new modeling study suggests an impressive impact of the COVID-19 vaccine on the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) attack rate (the risk of getting COVID-19), hospitalizations, and infections, even with no protection against infection. The results would also be improved if the vaccine prevented infection as well.
The COVID-19 pandemic refuses to die down, even though many countries worldwide have imposed lockdowns, including school and workplace closures and social distancing. These have closed down vast numbers of businesses in affected regions and the disease itself has claimed over 1.6 million lives globally. The second wave has already hit many parts of the world, making a vaccine an urgent priority.
The World Health Organization (WHO) has published its target product profile (TPP) for a COVID-19 vaccine, which includes criteria such as a population-based efficacy of 70% or over.
The recently approved Pfizer-BioNTech and Moderna vaccines have been reported to have over 90% efficacy, not against infection but against symptomatic disease. Health Canada, the national health authority for Canada, has already authorized the distribution of the former vaccine, and several others are being reviewed for approval.
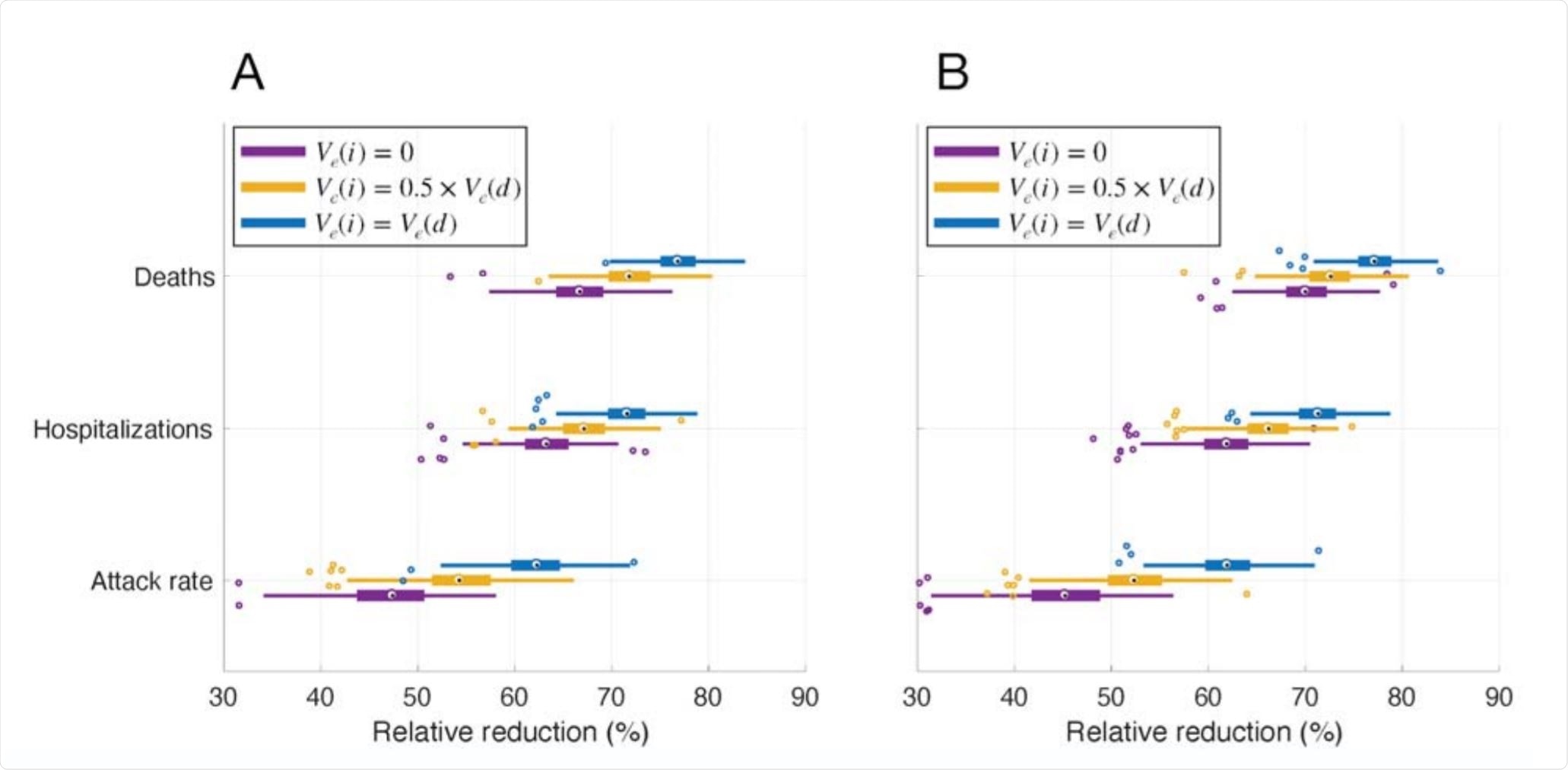
Projected relative reduction of attack rate, hospitalizations, and deaths in vaccination scenarios with a vaccine roll-out of 30 vaccine doses per 10,000 population per day. Image Credit: https://www.medrxiv.org/content/10.1101/2020.12.10.20246827v1.full.pdf

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Projecting Vaccine Impact
The current study seeks to establish the potential impact of such vaccines on the population when distributed in a prioritized manner. It appeared as a preprint on the medRxiv* server in December 2020.
The study was based on agent-based modeling, covering disease transmission. The vaccine distribution was implemented in an age-specific distribution borrowed largely from previous influenza outbreaks and the 2009 pandemic of H1N1.
Healthcare workers, older adults and those with other coexisting illnesses were on the priority list for vaccination to protect them against severe disease. Next came those aged 18-64 years, to break the chain of transmission.
Some of the relevant parameters include the disease's natural history, implemented as susceptible, latent infection, asymptomatic, presymptomatic, symptomatic, recovered non-infectious, and dead.
The daily number of contacts for each person was also assigned based on appropriate distributions.
The infectivity at each stage was implemented as 11%, 44%, and 89% in the asymptomatic, mildly symptomatic, and severely symptomatic, respectively, compared to the presymptomatic stage. The outcomes were the attack rate and adverse outcomes in Ontario, Canada.
Vaccine Parameters
The vaccine was assumed to be given in two doses, positioned at an interval of 21 or 28 days, to 40% of the target population.
Vaccination would be performed for 30/10,000 population per day in Ontario. With immunization occurring six days a week, vaccine coverage of 40% would appear in 40 weeks. Children were not vaccinated.
According to clinical trial data, the vaccine efficacy after the first dose was estimated at 52% and 95% after two doses. If the vaccinated individuals tested positive for COVID-19, the same protection was estimated against severe disease. The vaccine was estimated to assume protective efficacy from 14 and 7 days after the first and second dose, respectively.
The researchers used different scenarios to model the vaccine efficacy in preventing infection. This included zero protection, low efficacy against infection (only half of the protection against COVID-19), and equal efficacy against infection and disease. Reduced efficacy was assumed for people who were older or had other medical conditions. The vaccine was assumed to effectively reduce the disease's spread, the chances of symptomatic disease, and disease severity. They also assumed a 5% pre-existing immunity to the virus.
Each population of 10,000 was treated as if one individual had a latent infection, with the subsequent incidence of infection, hospitalizations, and deaths.
High Reduction in Attack Rate, Hospitalizations and Deaths
The researchers found that in the absence of a vaccine, and with current non-pharmaceutical interventions in place, the attack rate was projected to be 5.5%. Following vaccination, the outbreaks were smaller and more limited. The attack rate was reduced by ~45% for a vaccine which protected only against disease, to 62% after vaccination, assuming equal efficacy against infection and disease.
In the first case, hospitalizations and deaths went down by ~64% and 70%, respectively, following vaccination. In the second scenario, the reduction was by ~71% and 77%. In both scenarios, the highest benefit was in reduced mortality. No significant difference was seen with a 21- vs. 28-day interval between the two vaccine doses.
The number of hospital bed-days was also cut, even if the vaccine was not effective against infection. When the efficacy against infection was 50% lower relative to the protection against disease, and when it was equally effective against both, the reduction was even more significant, to ~47 and ~41 bed-days, respectively. Even without efficacy against infection, a vaccine could produce a 60% reduction in severe disease and mortality, as long as it is highly effective against disease and poor outcomes.
What are the Implications?
The uptake of the vaccine depends on multiple factors, logistical and otherwise. Dropouts from the vaccine program were not considered.
Vaccination, even with a vaccine that offers limited protection against infection, could have a large impact on reducing hospitalizations and deaths in Ontario.”
Therefore, this study supports the central role of vaccination in the current pandemic. This holds true even though NPIs will continue to be required to keep the rates of severe and lethal COVID-19 low before population immunity increases to high levels.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources