Researchers from Cornell University, USA, have modeled the effect of vaccination on the spread of COVID-19 disease. They suggest that vaccinating healthcare workers first followed by people who have many social interactions, such as grocers and airline cabin crew, will help reduce transmission. The research is published on the preprint server medRxiv*, prior to peer review.
Vaccines have been an essential strategy in the fight against COVID-19 caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Many vaccine candidates have been developed, with one receiving emergency use authorization and several others close to receiving authorization.
Pfizer and Moderna have reported vaccine efficacies of more than 90%. Astra Zeneca reported its vaccine candidate to have an efficacy of 62% for the group that received two doses and 90% in the group that received half the dose.
The recent approval of a vaccine for use against COVID-19 in the United Kingdom and the US, and pending approvals in India and many other countries, heralds a positive turn. Several other vaccines are in the final stages of clinical trials, with more approvals possible in the near future.
However, with people starting to be vaccinated, several questions arise, such as who should be vaccinated first to stop transmission quickly and how quickly after vaccination, people can go about their everyday lives.
Researchers at Cornell University and Weill Cornell Medicine used a mathematical model developed previously by the researchers to answer these questions. The model calculates the rate of emergence of new cases as a function of the spreading rate, the probability of target susceptibility, and the number of cases. They solved the model for a hypothetical city with a population of 300,000.
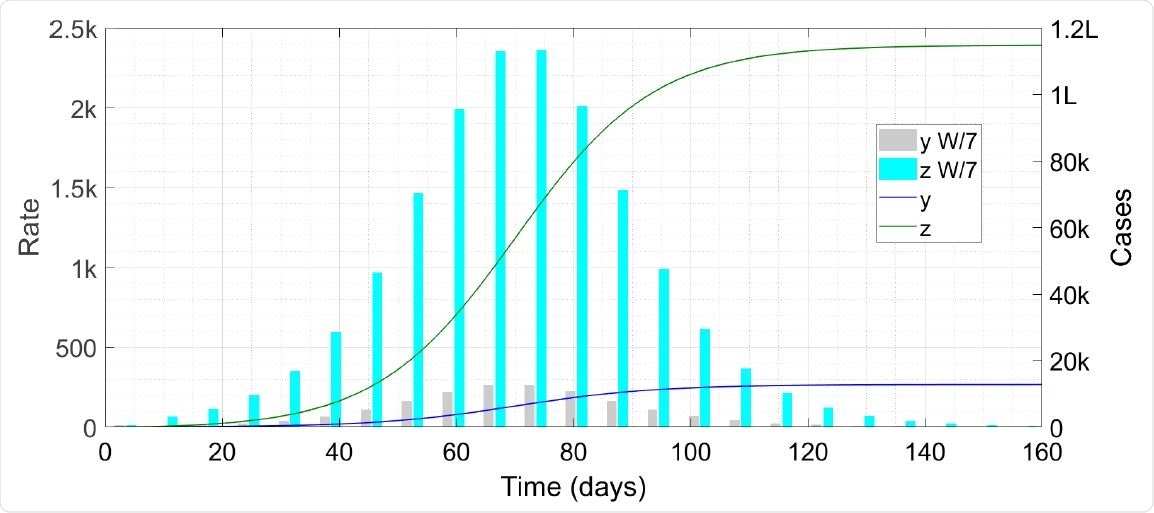
Time trace of the epidemic without vaccination. The symbol ‘k’ denotes thousand, ‘L’ hundred thousand and ‘W/7’ weekly cases scaled down by a factor of seven.
Who should get vaccinated after healthcare workers?
The first in line to get the vaccine will be healthcare workers, after that, the question is who's next in line?. To answer this, the authors assumed 10% of the population has a significantly higher interaction rate than the other 90%, such as shopkeepers, restaurant workers, and bus drivers.
The model showed that preferentially vaccinating the fraction of the population in the high interaction class can result in faster termination of the disease and lower infection counts by a factor of around 4.5 compared to a case where the high interaction class of population is not preferentially vaccinated.
That older people should be next to get the vaccine is something most policy-makers are thinking of. "While this reflects a noble sentiment, the maths might recommend a more balanced approach," write the authors. The elderly are expected to be in the low-interaction population, so it "might be more prudent to spend say half the doses on these people and the other half on high-interaction people, whatever their age."
Answering other questions
The next question the authors looked at was if people who have been vaccinated can take off their masks and go about their normal activities. For this, they assumed that the interaction rate of a person in the low interaction class goes up immediately after vaccination.
Their analysis indicates that people who have been vaccinated can return to everyday life without masks because the number of cases, in that case, would be minimal. They suggest removing restrictions for people who have been vaccinated and providing some form of identification to such people to make it easier when allowing relaxations.
Regarding the need for repeated doses of vaccines, the authors write that it may be possible that multiple doses are required over time to retain immunization as long as the virus is around. However, there are too many unknowns currently to determine if the disease can be eradicated entirely.
Another scenario the authors looked at was how hesitancy to get the vaccine may affect the efforts to reduce or eliminate COVID-19. The model suggests this may not be a big concern if there a proportion of people who resist being vaccinated.
If a vaccine is said to be 90% efficacious, according to the model, the probability of being protected from the virus will be around 90% and not a much lower number. So, the current numbers of the efficacy of the different vaccines are probably close to what would be seen in a challenge trial or the real world.
One of the model's limitations is that it uses a two-component interaction-structuring, and reality may perhaps be modeled better by a three- or six-component model. However, the key conclusions of the model, of preferentially vaccinating people who have a large number of interactions and allowing vaccinated people to resume normal life, seem robust and qualitatively intuitive, according to the authors.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.