Researchers in the UK have presented data from the latest in a series of community surveys assessing the prevalence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in England.
SARS-CoV-2 is the agent responsible for the coronavirus disease 2019 (COVID-19) pandemic that recently led to a second lockdown in the country between 5th November and 2nd December 2020.
The REal-time Assessment of Community Transmission-1 (REACT-1) study monitors the spread of SARS-CoV-2 through repeated rounds of community-based polymerase chain reaction (PCR) testing of self-administered nose and throat swabs.
Researchers from Imperial College London and Lancaster University have now provided updates from the latest survey (round seven), where swab collection began on 13th November and ended on 3rd December.
The results suggest that the second lockdown was accompanied by an overall decline in the national prevalence of SARS-CoV-2.
“This has helped to offset the large rises in prevalence observed during October 2020,” says Paul Elliott and colleagues.
However, the decline in prevalence was highly variable or “heterogenous” across the country.
For example, the researchers found evidence of a recent increase in London – particularly in the south and south-east of the city. In contrast, prevalence fell in the West Midlands and East Midlands.
The focus of infection has also shifted from people aged 18 to 24 years to school-aged children, particularly those aged 13 to 17 years, where prevalence is around 1 in 50.
The researchers say continued vigilance is needed to reduce the infection rate until herd immunity can be established through vaccination.
A pre-print version of the paper is available on the medRxiv* server, while the article undergoes peer review.
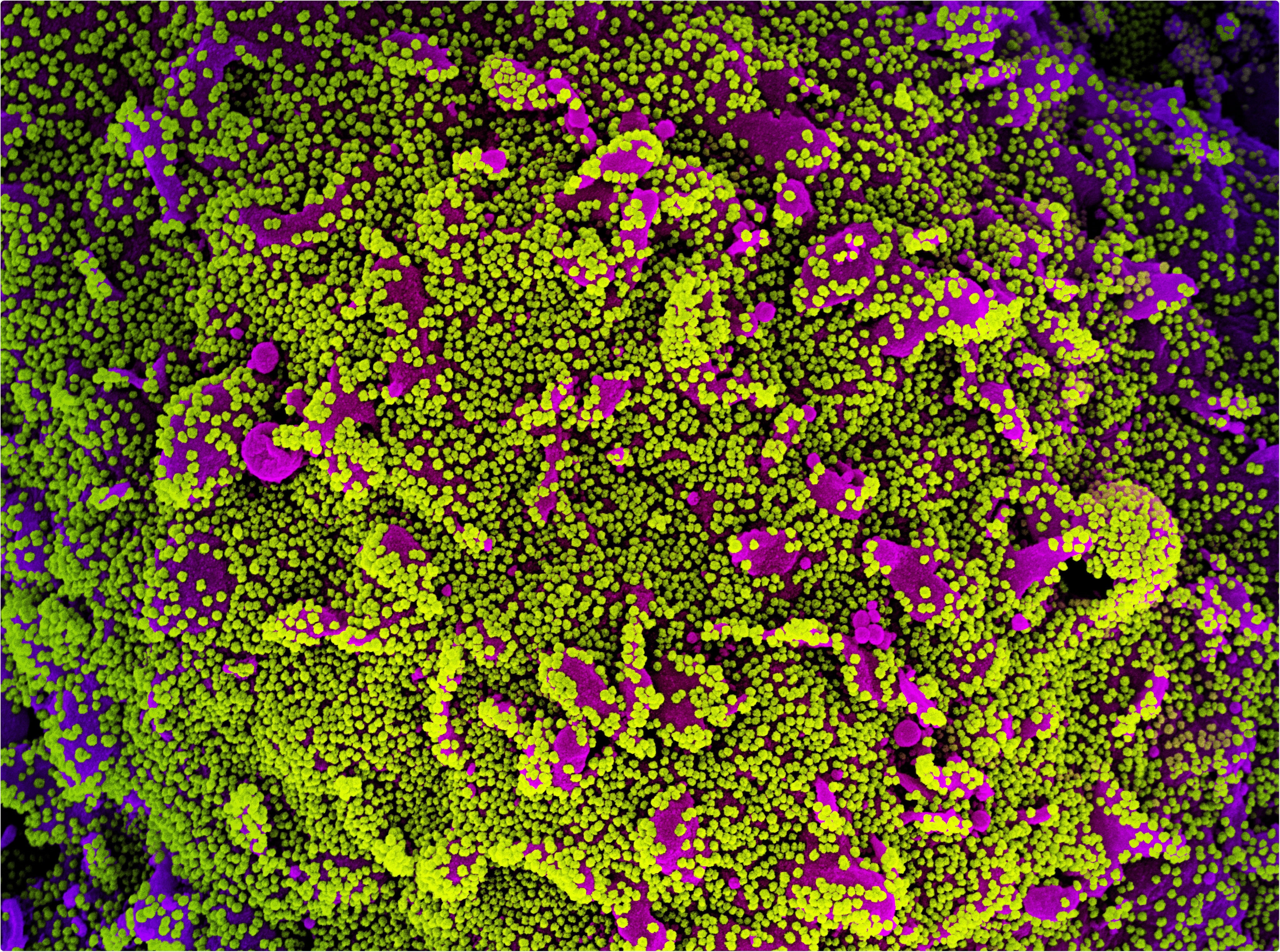
Colorized scanning electron micrograph of a cell (purple) heavily infected with SARS-CoV-2 virus particles, isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Estimating SARS-CoV-2 prevalence in England
In England, a rapid increase in the number of COVID-19 cases through October led to a four-week national lockdown on 5th November, which the country exited on 2nd December.
REACT-1 is a series of community surveys that has been monitoring the spread of SARS-CoV-2 on an approximately monthly basis since the latter period of the first lockdown in May 2020.
The prevalence of SARS-CoV-2 is estimated nationally, regionally, sub-regionally, and by socio-demographic factors and other characteristics. Time trends and reproduction numbers (R) within and between rounds are also estimated using exponential growth models.
The seventh round of data collection began on 13th November and ended on 3rd December, therefore covering most of the second national lockdown (5th November to 2nd December).
What did round seven find?
Of 168,181 swabs tested, 1,299 were positive for SARS-CoV-2, giving a prevalence of 0.94% or 94 per 10,000 people.
This compares with a prevalence in the sixth round (16th October to 2nd November), of 1.30%, representing a fall of 28%.
This reduction in overall prevalence between the previous and most recent rounds suggests that the second lockdown appears to have been effective at reducing the infection rate, albeit less effective than the first lockdown.
There were significant regional differences in prevalence
Overall, the estimated national R number during round seven was 0.96.
However, the regional estimates of R numbers indicated countrywide heterogeneity.
For example, while prevalence fell in the West Midlands, it increased in London and leveled out in other regions.
During the second half of round seven, prevalence increased from 0.98% to 1.21% in London, from 1.17% to 1.39% in Yorkshire and The Humber, and from 0.72% to 1.26% in the North East.
The highest prevalence in London was observed in the east and south-east of the city, where it also seemed to be increasing the most. Prevalence rates also appeared to be increasing in the East (Essex) and South East (Kent).
In the West Midlands, the prevalence halved, falling from 1.55% to 0.71% and in the East Midlands it fell from 1.27% to 1.04%. In the North West, the prevalence dropped from 1.08% to 0.92%.
The estimated R numbers ranged from 0.60 in the West Midlands to as high as 1.27 in London.
Reasons for the regional heterogeneity are not clear, but may involve the strictest containment measures being introduced in large parts of northern regions in the form of tiering systems since before lockdown, says Elliott and the team.
“Some of the recent improvements may therefore reflect the combination of these prior measures and lockdown,” they write.
What about prevalence among different age groups?
Analysis of prevalence by age group showed that levels were the highest among school-aged children. Among those aged 5 to 12 years, the prevalence was 1.70% and among those aged 13 to 17 years, it was 2.04% or approximately 1 in 50.
“The previous focus of infection, which was in the 18 to 24 year-olds, had shifted to school-aged children, especially those in 13-17 year-olds,” writes the team.
“Continued vigilance is required”
The researchers say that taken together with other available data. These regionally stratified data provide a more complete picture of how the COVID-19 epidemic is evolving over time.
While the prevalence of SARS-CoV-2 swab-positivity declined nationally, it did not decline uniformly over time or by geography, says the team.
“In particular, we found evidence for a recent rise in London and a flattening off elsewhere.”
“Continued vigilance is required to reduce rates of infection until effective immunity at the population level can be achieved through the vaccination program,” concludes Elliott and colleagues.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.