The coronavirus disease 2019 (COVID-19) pandemic has caused enormous harm to human health and life expectancy, as well as to the economy worldwide. The pandemic has also highlighted healthcare inequalities.
Strict limitations on mobility and social interactions closed down workplaces, schools, and retail stores, leading to economic disruption. While this succeeded in slowing down the spread of the virus, it simultaneously made business impossible or unprofitable in many ways.
The resulting economic recession is reflected in the ~11% dip in the gross domestic product (GDP) in the second quarter of 2020, among countries in the OECD (Organization for Economic Co-operation and Development). Unemployment rates increased by 5.3% and 8.6% in the first and second quarters of 2020, respectively.
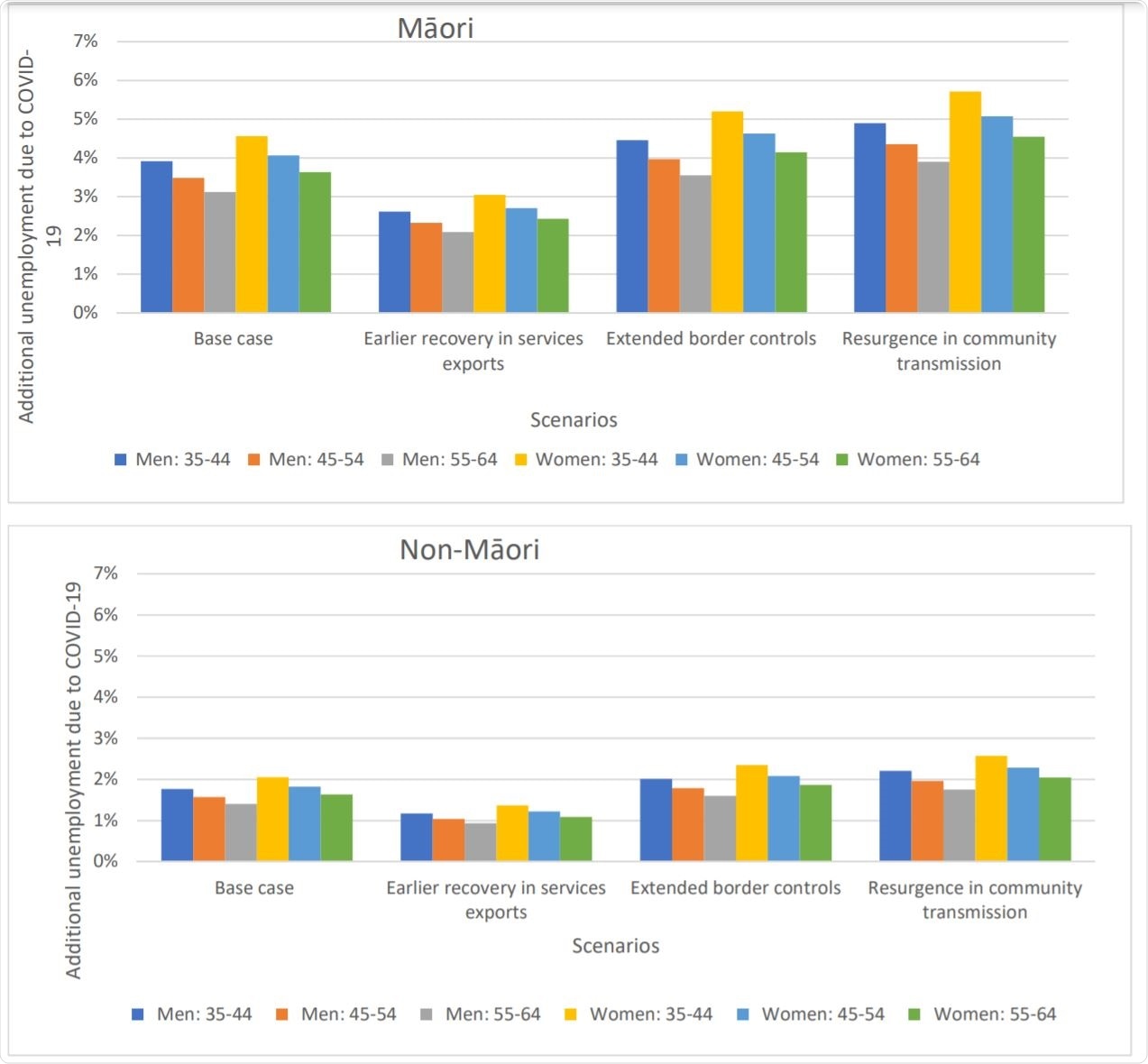
Scenarios around the COVID-19 pandemic related additional absolute unemployment rates in 2021 used in the BODE3 CVD model by age, sex and ethnicity in NZa,b,c,d. Image Credit: https://www.medrxiv.org/content/10.1101/2020.12.15.20248284v1.full.pdf

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Unemployment causes increased cardiovascular disease
Unemployment and economic depression are known to increase the risk of cardiovascular disease (CVD). Lockdowns increase job insecurity, stress, and loneliness.
These established facts spurred the current study of the effects of the pandemic on health and economics, particularly among the aboriginal Maori population, which is known to suffer disproportionately from CVD and health inequalities.
New Zealand estimates of unemployment
New Zealand (NZ) took strict and repeated action against the pandemic, aiming to eliminate the virus. This restricted COVID-19 related deaths to only 25 but affected international trade, caused the loss of international students, and impacted local business.
The low number of infections led to the use of indirect measures to estimate the effect of COVID-19 on health, such as the increase in CVD caused by unemployment following the pandemic.
The NZ government described the pandemic as a ‘once in a century’ public health disruption that has caused a ‘highly uncertain’ effect on key economic outcomes. The NZ Treasury presented its estimates of unemployment rates under four different scenarios.
One was the base case, where border restrictions were expected to be eased in part in July 2021 and fully in January 2022. The exports of services would show a relative decrease of 13% in December 2024 vs. December 2019.
Secondly, if services exports recovered earlier, they would still suffer a relative decline of 4%. If border controls failed to be relaxed completely, on the other hand, the relative fall would be 35%. Finally, if community transmission went up, the GDP would be 1% less than in the base case, despite unchanged border restrictions and services exports.
The Treasury estimated unemployment rates ranging from 7.7% to 9%, depending on the level of restrictions. It also presented an increase in unemployment even at five years after the pandemic in all visualized scenarios.
Unemployment-related CVD burden
The researchers used this data, based on four different scenarios of COVID-19 response, to create a model adjusted for age, sex, and ethnic origin. They implemented the health burden due to unemployment in terms of CVD mortality and morbidity alone, using a large study on the relationship between a rise in unemployment rates among middle-aged men and CVD mortality. The study found that the latter rose by 0.85% with every 1% rise in unemployment, both relative to baseline rates.
Immense CVD-related health loss
The current study extended this effect size in a linear fashion and attributed the increase in mortality to an increase in CVD incidence. The researchers found that the estimated health loss related to CVD in the base scenario, with the best estimates, was -30,000 health-adjusted life years (HALYs), with 10% of this loss being experienced in the five years immediately following the pandemic and more than 50% over the next 20 years.
With alternative scenarios, such as an earlier recovery in international tourism and international education, or the second rise in community transmission, the CVD-linked decline in health would be ~23,000 and ~37,000, respectively.
Maoris experience four-fold higher CVD-related health loss
In the case of the Maori community, the health loss in terms of CVD would be from -7,700 and -13,000, compared to -15,700 to -26,600 for the non-Maori population. The former had 3.7 times greater health loss compared to non-Maoris, as shown by the 50 vs. 13.5 HALYs loss per 1,000 people.
When stratified by sex, the change in HALYs per 1,000 people was ~96% among Maori men, of ages 35-64 years, but only ~25% among non-Maori men in this age group. The equity ratio was four-fold in favor of non-Maori men.
Similarly, the loss among Maori women was ~9 per 1,000 compared to ~3 for non-Maori women, in this age group, with an equity ratio of 3.2 in favor of the latter.
If examined by age-group, the change in HALYs per 1,000 was between -93 to -103 for Maori men aged 35-44, 45-54, and 55-64 years, while it remained between 20 and 27 for non-Maori men in these groups. The corresponding equity rates for each group ranged from 3.2 to 4.5 in favor of the latter.
For Maori and non-Maori women in these groups, the corresponding changes ranged between ~10 and -36, and 1.5 to -8.5, respectively. Here, the equity ratios favored the latter by 4.3 to 7 times.
The highest level of disparity in health was reflected in the sixfold increase in CVD burden among Maori women aged 45-54 years, in all scenarios, compared to non-Maori women.
The higher health cost burden
Depending on the scenario, the NZ health care system would also suffer a higher health cost due to the additional CVD burden, between NZ$303 million to 503 million (US$209 million to 346 million) in 2019 values. Here again, the burden was shared between 10% in the five years of the forecasting period and over 60% in the next 20 years.
Implications and future directions
Further refinements are necessary to adjust for other causes of CVD and all-cause mortality, such as sedentary behavior during the lockdown, with increased consumption of tobacco, fast food, and alcohol. On the other hand, lower incomes might result in reduced rates of consumption of these substances and foods due to reduced buying power. More data will be required.
A possible negative impact of the lockdown on healthcare delivery should also be investigated. The study also excluded people above the age of 65 as only a minority of these are in active employment.
Despite these limitations, the authors suggest that governments should prevent such health losses and increased severity of health inequities by active intervention in job creation policies and programs. These could target disadvantaged communities to bring their unemployment rates nearer to those of non-Maoris.
Active education of the population on the risk of CVD and measures to mitigate this risk should also be on the agenda.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources