As the coronavirus pandemic continues to wreak havoc across the globe, there is a dire need for effective and safe therapeutics and vaccines. Overall, the pandemic has infected more than 90.87 million people and taken more 1.94 million lives.
Previous studies have shown the impact of vitamin D supplementation on coronavirus disease (COVID-19) patients. Further, vitamin D deficiency has been linked to poor clinical outcomes in patients infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19.
A team of researchers at the University of Medicine and Pharmacy of Craiova in Romania and the National and Kapodistrian University of Athens in Greece aimed to determine the role of key biological variables that could interplay with virus spread and severity. The team found that vitamin D may turn into an effective adjuvant to reduce the impact of the coronavirus pandemic, particularly in regions where vitamin D deficiency is prevalent.
The study
In the review, published in the International Journal of Molecular Medicine, the researchers aimed to unravel the roles of vitamin D status and melanin during COVID-19 infection.
The researchers discussed how vitamin D status and melanin on the skin interplay to determine a patient’s clinical outcome. Given the supportive role of vitamin D in immune responses against respiratory viruses, including SARS-Cov-2, the team wanted to know how vitamin D status can influence clinical outcomes in patients with COVID-19.
Since vitamin D results from endogenous skin production after being exposed to ultraviolet solar radiation, skin pigmentation may also play a role in non-white ethnic variations of COVID-19, since melanin can reduce the capacity of the skin to effectively absorb sunlight and synthesize vitamin D3.
Hence, the team wanted to explore the evidence related to vitamin D status and melanin pigmentation on the skin that may lead to clinical implications on the course of COVID-19 disease and patient clinical outcome.
Vitamin D and COVID-19
The reports on clinical outcomes and risk factors for disease and death tied to COVID-19 are increasingly emerging. Though there are differences in countries and populations, several factors may account for this discrepancy. These include general health, age distribution, and socioeconomic status.
Since the pandemic started, many studies have shown the link between vitamin D deficiency and a higher risk of developing severe COVID-19 and of COVID-19-related mortality. Further studies have noted that taking Vitamin D can reduce a patient’s chances of severe SARS-CoV-2 infection.
Since vitamin D plays a pivotal role in the clinical outcomes of patients with COVID-19, the research study focused on the potential impact of vitamin D status on COVID-19 outcomes.
The researchers noted that evidence suggests that the vitamin D endocrine system is involved in several biologic processes and pathways, which affect not only musculoskeletal health but also the emergence of other diseases. For instance, it has been known that vitamin D status may affect outcomes of respiratory and infectious diseases, hence, hinting at the role of vitamin D in the immune system.
Vitamin D has also been tagged in its many roles in immunity, inflammation, and epithelial repair. Specifically, 1,25-dihydroxyvitamin D3 (1,25(OH)2D3), the active metabolite of Vitamin D has long been recognized to contain immune regulatory properties. Many past studies have demonstrated that vitamin D can contribute to the defense against viral infections, specifically acute respiratory tract infections.
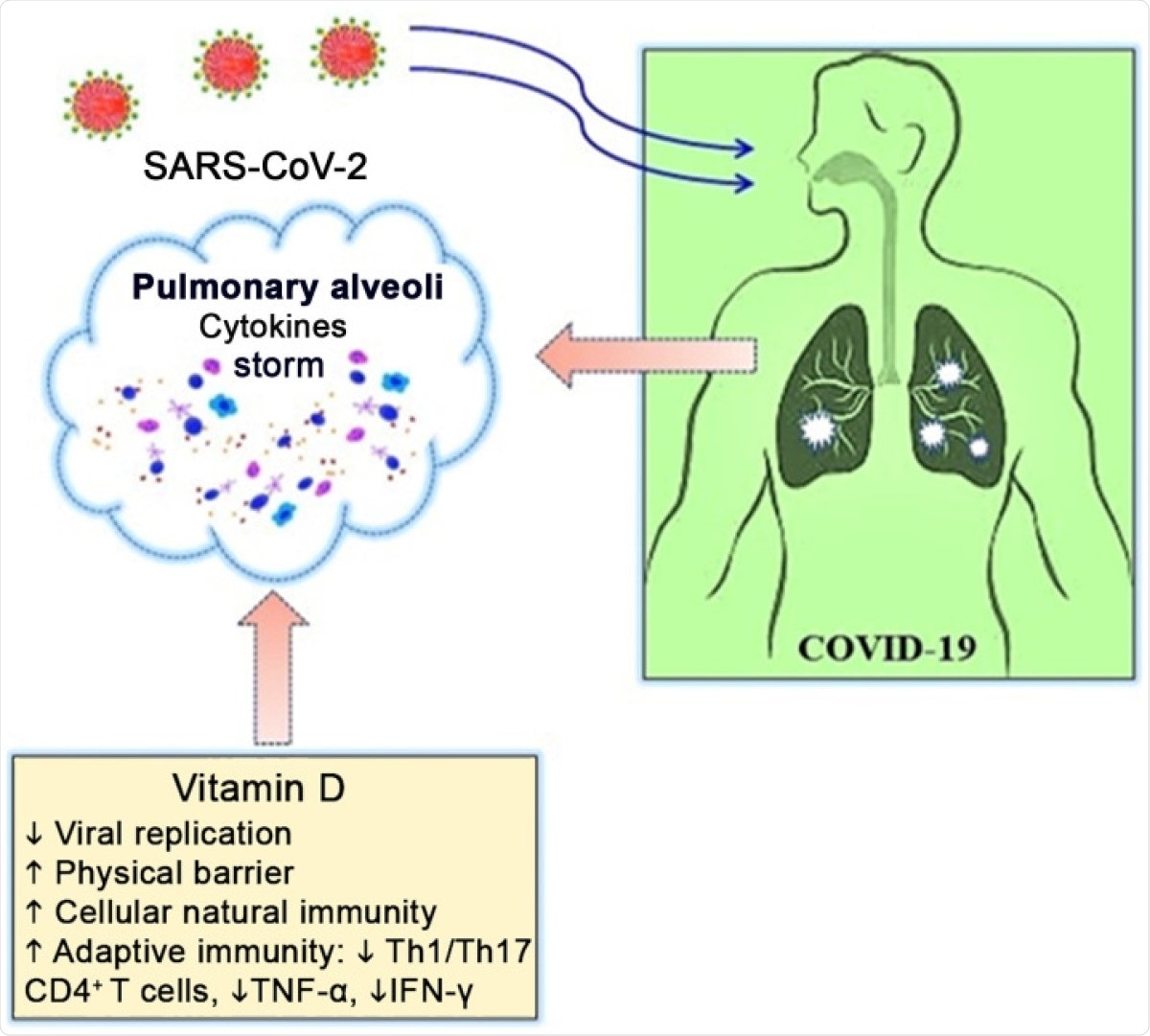
Potential antiviral mechanisms of vitamin D in COVID-19. COVID-19, coronavirus disease 2019; IFN-γ, interferon-γ; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; Th, T helper; TNF-α, tumor necrosis factor-α.
Melanin pigments are drivers of human pigmentary status. In the course of the coronavirus pandemic, there is a disparity in the severity of COVID-19 illness in some racial groups.
In the study, the researchers noted that increased melanin levels in the skin are known to be inversely proportional to the vitamin D status. Thus, this may account for the observed differences in vitamin D deficiency.
Fair-skinned people only need about 20 to 30 minutes of midday sunlight exposure about 2 to 3 times a day to get a sufficient amount of vitamin D. On the other hand, darker skin people may need higher weekly ultraviolet ray doses to meet their vitamin D needs.
In summary, the review aimed to expand the current knowledge of vitamin D status and melanin and their effects on COVID-19 outcomes. The team noted that vitamin D may be an effective way to reduce the impact of COVID-19 on high-risk populations.
Given that vitamin D is a safe, inexpensive, and widely available agent, even in countries with limited resources, vitamin D inadequacy is an easily modifiable risk factor,” the team explained.
Overall, the researchers suggest that vitamin D may prove an effective adjuvant to vaccines and antiviral therapeutics in the fight against COVID-19.