Researchers in Israel have conducted a study showing that increased hospital load due to rising coronavirus disease 2019 (COVID-19) cases resulted in higher COVID-19-related mortality, despite hospitals not exceeding their defined threshold for meeting patients' treatment needs.
The team attributes the increased mortality rate to the rapid influx of new cases over short time periods leaving healthcare systems overwhelmed and under-resourced.
Malka Gorfine and colleagues found that even when patient load was only moderately heavy, the rate of in-hospital COVID-19-related mortality significantly increased, compared with periods of lower patient load.
They further showed that this increased mortality could not be attributed to changes in the patient population, such as older age or increased clinical vulnerability.
The team says the findings highlight that even in countries where healthcare systems do not reach the defined threshold for being unable to meet patients' treatment needs, the increase in workload may lead to rises in patient mortality.
The study emphasizes the importance of quantifying excess mortality to define an appropriate level of caring capacity, inform timely healthcare policies and allocate the necessary resources, say the researchers from Tel Aviv University, the Weizmann Institute of Science in Rehovot, Rambam Health Care Campus in Haifa, and Israel Institute of Technology in Haifa.
A pre-print version of the research paper is available on the medRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Hospital overwhelmed by increased workload
The COVID-19 pandemic has led to many healthcare systems quickly becoming overwhelmed by an increased workload.
"The heavy workload imposed on hospital services might have negatively affected patients' outcomes and exacerbated mortality rates," said Gorfine and colleagues.
In Israel, the first COVID-19 case was identified on 2nd February 2020. The country's ministry of health (MOH) responded by gradually introducing social distancing measures to help curb the pandemic's spread.
Following the relaxation of these measures in May, the number of new cases substantially increased, and by 10th September, the country had the highest rate of COVID-19 cases per capita globally.
A national lockdown was imposed in mid-September, but its relaxation during October led to a further rise in cases and a subsequent third lockdown in January 2021.
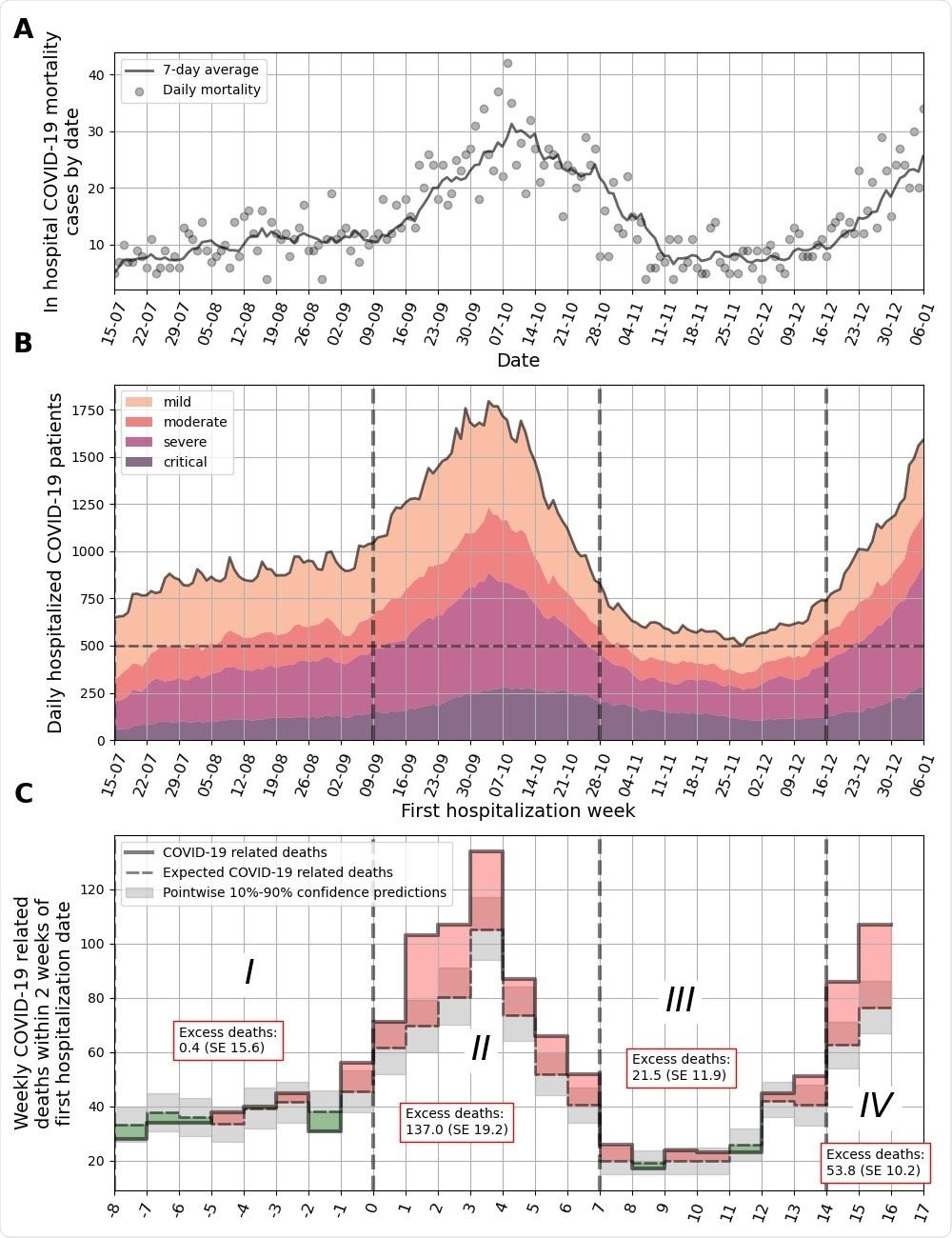
In hospital COVID-19 related mortality cases by date. Daily mortality is marked by gray circles, and a 7-day average is plotted as a solid line. B. Number of COVID-19-related hospitalizations by day in all hospitals in Israel. Colors depict different clinical states. A threshold of 500 severe and critical patients per day is presented by a dashed horizontal line. Dashed vertical lines separate weeks that are over/under this threshold. C. COVID-19 related deaths for sets of patients that were first hospitalized in different weeks. Observed deaths for each week are marked by a solid line. Expected deaths as predicted from the model are marked in dashed black line. Monte-Carlo-based pointwise 10%-90% confidence predictions are marked in gray. Weeks in which excess deaths were observed ( positive difference between true and expected curves) are filled in red; and weeks in which deaths were overestimated ( negative difference between true and expected curves) are filled in green. X-axis is marked by the week number. Abbreviations: SE - Standard Error
What did the researchers do?
The researchers investigated the effects of increased hospital load due to rising COVID-19 cases on the mortality rate among patients hospitalized with the disease.
They conducted a nationwide study using the records of 19,336 COVID-19 patients (aged a mean of 59 years) hospitalized in Israel between 7th July 2020 and 6th January 2021.
Excess mortality was assessed using a model previously developed for predicting patient mortality based on daily information on disease course. Disease severity was classified as mild (signs and symptoms of COVID-19 such as fever, cough); moderate (evidence of pneumonia); severe (advanced breathing problems) or critical (requiring ventilation or presence of multiorgan dysfunction).
Patient data also included information on age, sex, hospitalization date, and clinical outcome (death or hospital discharge from hospitalization).
Data were divided into four time periods: period 1 covered hospitalizations from 15th July to 8th September; period 2 from 9th September to 27th October; period 3 from 28th October to 14th December and period 4 from 15th December to 6th January.
Excess mortality was estimated by comparing the observed mortality and the model's predicted mortality.
What did the study find?
The researchers showed that patient mortality significantly exceeded the model's predicted mortality during period 2 (9th September to 27th October) and period 4 (15th December to 6th January).
During these periods, the daily number of severe and critical patients exceeded 500, which classifies as a moderately heavy patient load, according to the MOH definitions. During periods 1 and 3, the daily number of severe and critical patients was between 250 and 500, which classifies as a lower patient load.
"The threshold defined by policymakers in Israel as an upper bound in which the healthcare system won't be able to treat patients adequately was 800 severe and critical patients," writes the team.
However, under the moderately heavy load (periods 2 and 4), the in-hospital rate of COVID-19-related mortality significantly increased, compared with during the periods of lower patient load (1 and 3).>
The researchers point out that this higher mortality rate cannot be attributed to changes in the patient population during periods of heavier load.
"The model adjusts for age, sex and clinical state upon the first day of hospitalization, and the predictions, therefore, take these differences into account," they write.
Furthermore, the increase in observed mortality occurred despite clinicians becoming more experienced in treating COVID-19 and acquiring an improved understanding of pharmacologic approaches over time.
The team proposes that the excess mortality during periods 2 and 4 is most likely due to the rapid increase in the number of COVID-19 hospitalizations, which may have resulted in insufficiency of healthcare resources that negatively affected patient outcomes.
"Our work emphasizes that even in countries in which the healthcare system did not reach a specific point defined as insufficiency, the increase in hospital workload was associated with quality of care and patient mortality," says Gorfine and colleagues.
"In addition, our study highlights the importance of quantifying excess mortality in order to assess the quality of care, and define an appropriate carrying capacity of severe patients in order to guide timely healthcare policies and allocate appropriate resources," they conclude.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Gorfine M, et al. Hospital load and increased COVID-19 related mortality - a nationwide study in Israel. medRxiv, 2020. doi: https://doi.org/10.1101/2021.01.11.21249526, https://www.medrxiv.org/content/10.1101/2021.01.11.21249526v1
- Peer reviewed and published scientific report.
Rossman, Hagai, Tomer Meir, Jonathan Somer, Smadar Shilo, Rom Gutman, Asaf Ben Arie, Eran Segal, Uri Shalit, and Malka Gorfine. 2021. “Hospital Load and Increased COVID-19 Related Mortality in Israel.” Nature Communications 12 (1). https://doi.org/10.1038/s41467-021-22214-z. https://www.nature.com/articles/s41467-021-22214-z.