Many patients with coronavirus disease 2019 (COVID-19) have shown neurological complications, leading to scientific interest in the role played by its causative pathogen, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), in brain inflammation. A new preprint that appeared on the medRxiv* server described the absence of neuroinflammation in cerebrospinal fluid (CSF).
Several earlier CSF studies have not found consensus on how and in what ways COVID-19 can be associated with related neurological symptoms. Some researchers have found anti-SARS-CoV-2 spike immunoglobulin G (IgG) antibodies in several such patients with encephalopathy; others have claimed to find inflammatory markers or signs of neuron damage.
Study details
The current study looked specifically for features of neuronal inflammation, antibodies to the virus, and viral RNA. They also compared the CSF from COVID-19 patients with neurological features with that of non-COVID-19 patients with stroke, neurological infections, and inflammations of the nervous system. They aimed to identify any common pathways underlying these symptoms.
The researchers carried out a cross-sectional study on 18 adult COVID-19 patients, who had neurological features, and 14 healthy controls, along with 68 patients without COVID-19 but with neurological disease. The median age in the COVID-19 group was 56 years, and over half were male.
Of the 18 patients, 16 had a diagnosis of COVID-19 based on reverse transcriptase-polymerase chain reaction (RT PCR) testing, and two based on positive serology. Five and eight patients had severe and critical disease, respectively, while four had moderate disease. Four of them succumbed to the illness.
Neurological manifestations in COVID-19 comprised seven cases of stroke, six with encephalopathies, and five with headaches or other symptoms. A third of them (six patients) had COVID-19 hyperinflammatory syndrome (C-HIS), of whom four had encephalopathy. The median time from the onset of COVID-19 to neurological symptoms was less than a day. In half of the 18 patients, the initial presentation included neurological manifestations.
Six of them had three or more underlying chronic conditions, with nine of them having one or more such conditions.
Of the controls, there were only 14 healthy individuals, while the rest had various infective or autoimmune conditions.
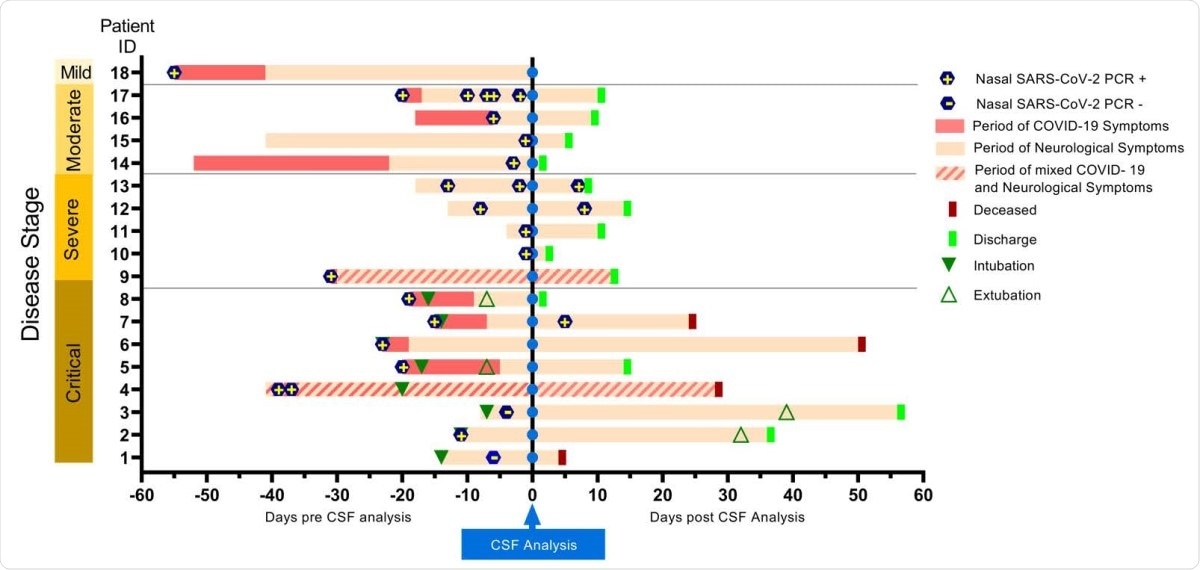
Timeline of clinical features in patients with COVID-19 with neurological complications. Temporal profile of COVID-19 and neurological symptoms as related with the time of CSF analysis (vertical blue line) for the 18 subjects included in the study. Patients were classified based on the NIH disease severity classification (56). Eight subjects presented with neurological symptoms as the first manifestation of COVID-19 (light pink bar), eight exhibited systemic illness symptoms preceding neurological symptoms (dark pink bar) and two presented with mixed neurological and systemic symptoms (diagonal stripes).
The CSF was collected from eight of the COVID-19 patients within eight days of the first positive RT-PCR, and after nine or more days in the other ten patients. None of the samples showed CSF pleocytosis, except in one, probably due to contamination with blood. CSF protein was high in eight patients, but in four of them it could be due to a falsely high number of red cells or the presence of stroke, or both. The CSF IgG index, as well as the CSF/albumin ratio, were normal in seven patients. In five patients, oligoclonal bands were tested for, in serum and in CSF.
SARS-CoV-2 in CSF
No COVID-19 CSF sample contained SARS-CoV-2 RNA, when tested by either of two methods. IgA and IgG antibodies against the virus spike protein were present in four and 13 of the 17 tested CSF samples, respectively. There was no correlation between IgG and severity of disease/neurological symptoms or the duration from either symptom onset or RT-PCR testing to CSF sampling. In six of the 13 IgG positives, no white or red blood cells were found. In the rest, there were more than 50 red cells due either to traumatic lumbar puncture or stroke.
Laboratory findings
There was no substantial variation in white cells or CSF protein between the COVID-19 patients in any of the three neurological categories, but when compared with healthy controls, CSF protein was lower in the COVID-19 headache group. Both white cells and protein were lower in COVID-19 patients than in patients with neuroinflammatory disease but without COVID-19.
Neuroaxonal degeneration markers
Neurofilament light chain was used as a marker of neuroaxonal damage, and was higher in COVID-19 patients with critical disease, and in the stroke group (with or without COVID-19), as well as in non-COVID-19 patients with acute encephalitis, autoimmune encephalitis and neuromyelitis optica among the controls.
Cytokine measurements
Within the COVID-19 group, the only increase was seen with TNFa. However, when compared with healthy controls, IL-6, TNFa, IL-10 and IL-12p70 were all increased in the COVID-19 stroke group. However, TNFa and IFNγ were still higher in patients with non-COVID-19 neuroinflammation or stroke. IL-10 and IL-12p70 were higher in critical COVID-19 CSF than in healthy controls, but also in the non-COVID-19 stroke group.
No significant difference was noted in CSF cytokines even in patients with C-HIS, relative to the healthy controls, but INFγ and IL-12p70 were lower in the former category compared to non-C-HIS cases. CSF IL-6 and serum IL-6 levels showed no association.
Acute phase reactants
CSF C-reactive protein (CRP) was associated with severe or critical COVID-19 and C-HIS, while CSF ferritin was associated with severe disease. However, the latter was linked to COVID-19 headache patients, and serum ferritin levels did not correlate with CSF ferritin levels. D-dimer levels were higher in non-COVID-19 patients. Cytokine levels were also not elevated and did not appear to be drivers of neuroinflammation in COVID-19.
What are the implications?
The researchers conclude that neuroinflammation is not supported by these findings. Instead, antibodies are robustly present, but not viral RNA. CRP in CSF was found to be related to severe or critical COVID-19, while neuroaxonal injury was also found to be present in both critical COVID-19 and in stroke patients. Stroke patients were marked by a selection of elevated cytokines, namely, IL-10 and IL-12p70.
The high IgG levels in COVID-19 CSF could be explained by increased permeability of the blood-brain barrier, or simple transfer due to elevated serum levels. They do not seem to be associated with disease severity, unlike earlier studies. This aspect deserves further study, especially in relation to the brain fog and other long-haul neurological manifestations following recovery from COVID-19.
This paucity of CSF inflammatory changes undermines the hypothesis that conventional neuroinflammatory or encephalitic processes play roles in the pathogenesis of the most common neurological complications associated with COVID-19.”
The majority of changes in CSF, indeed, are related to ischemia rather than neuroimmune disease, or the presence of active invasion by SARS-CoV-2. In this manner, therefore, this virus seems to be quite different from other neurotropic viruses like poliomyelitis or West Nile virus, that produce few signs but are overtly

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Garcia, M. A. et al. (2021). Cerebrospinal fluid in COVID-19 neurological complications: no cytokine storm or neuroinflammation. medRxiv preprint. doi: https://doi.org/10.1101/2021.01.10.20249014,https://www.medrxiv.org/content/10.1101/2021.01.10.20249014v1
- Peer reviewed and published scientific report.
Garcia, Maria A., Paula V. Barreras, Allie Lewis, Gabriel Pinilla, Lori J. Sokoll, Thomas Kickler, Heba Mostafa, et al. 2021. “Cerebrospinal Fluid in COVID-19 Neurological Complications: Neuroaxonal Damage, Anti-SARS-Cov2 Antibodies but No Evidence of Cytokine Storm.” Journal of the Neurological Sciences 427 (August). https://doi.org/10.1016/j.jns.2021.117517. https://www.jns-journal.com/article/S0022-510X(21)00211-2/fulltext.