The ongoing coronavirus disease 2019 (COVID-19) pandemic has caused many hundreds of thousands of deaths worldwide. England has been especially affected, with over 50,000 deaths documented by December 2, 2020. An informative new study by researchers at Imperial College London provides a mathematical model to help understand how the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen of (COVID-19), spread across England in the first two waves of the epidemic, and the effect of various interventions by the government. This could help policymakers to enhance the effectiveness of public interventions, “emphasizing the importance of acting fast to save lives.”
The model uses age-based structure and stochastic predictors of transmission to represent the spread of the virus in care homes, in-hospital, and in the community at large. Serological data was accumulated to allow the severity of the disease to be estimated by region and by age, with comparisons between the severity in people living in care homes vs similarly elderly people in the community, and to arrive at the total estimated size of the epidemic. The effects of the lockdown vs restriction of visitors to care homes were also studied quantitatively.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The team’s findings have been released on the medRxiv* preprint server.
The trend of the epidemic
The first death recorded to be due to COVID-19 in England was early in March 2020. After seven days, as the viral transmission became more obvious, control measures began to be mandated, such as self-isolation of people with a dry cough, for instance. A national lockdown came into effect on March 23, 2020. This reduced transmission to equal levels across all regions, indicating that it acted to restrict mobility with comparable efficacy across the country.
London was seen to have an earlier onset of the epidemic, at 15 days prior to the rest of the country, and to have a mortality of ~89 per 1,00,000 in the first wave. Conversely, the mortality for the rest of the country was ~71 per 1,00,000 in the rest of England, even though the population of London was younger with a smaller proportion in care homes, compared to the rest of England.
Care homes bore the brunt of the outbreak, contributing over one in five deaths by August 1, 2020. The first lockdown brought about some control of transmission rates in the community but the virus continued to wreak more damage in the care homes, with the peak of infection risk in these centers being somewhere between March 26 and April 12, 2020. The peak death rate in care homes occurred about two weeks later than in hospitals.
The lockdown in England was relaxed in stages from May 11, 2020, which led to a steady increase in viral transmission. By mid-August, the effective reproduction number (Reff) went above 1 all over the country.
A second wave began, necessitating new interventions such as the “Rule of Six” on public gatherings on September 14, 2020. Further restrictions were announced on October 14, to be implemented in tiers. These had some effect on viral spread but
could not contain it, so that the Reff continued to be above 1, leading to a second lockdown on November 5, until December 1, 2020. Schools and certain offices remained open throughout the lockdown this time, but the Reff was estimated to be 0.83, at the start. The researchers attribute this decrease from the expected Reff of 0.95 to population immunity, which reduced viral spread despite less stringent lockdown restrictions over this period.
Severity of the epidemic
The severity of the infection ranges from nil to fatal. The current study used data from over 17,000 patients hospitalized between March 18 and May 31, 2020, retrieved from the COVID-19 Hospitalisation in England Surveillance System (CHESS). When they studied the effect of the various medical interventions at different severity levels, they concluded that older patients, over the age of 65, were less likely to be admitted to intensive care units (ICU).
Since COVID-19 is likely to be more severe in older people, but this group, in common with those who are sicker, are likely to benefit less from ICU admission and ventilation, compared to putting them on oxygen therapy in a general ward. They remark, “Older and more severely infected patients may be directed to care on a general ward rather than admitted to ICU.”
Severity correlated with age in all regions except London, which had a median age of ~35 years vs ~40 years nationally. The infection fatality rates (IFR) for London and the rest of England were 0.9% and 1.25% respectively. Age alone could not explain the disparity, as those in London who were older than 80 years had an IFR of ~6% vs ~13% for the same age group in the Northwest of England.
The IFR first went up with increasing transmission, but fewer deaths in hospital occurred over time, so that by the end of the first wave the IFR was ~0.8%. The largest reduction occurred in London, at ~65%, and the least in the Northwest, at ~37%. Fewer hospital-associated deaths occurred among care home residents, but this was due to an increased proportion of fatalities within the homes themselves. Thus, the infection hospitalization ratio (IHR) among those aged 80 years or more was ~19% in care home residents, vs 51% in the community at large. On the other hand, the IFR in those of this age in care homes was ~40%, vs ~10% in the community.
Seropositivity mirrored the first wave with a two-week lag, but fell steeply in some places after the first wave, perhaps due to rapid waning of antibody titers.
Effect of non-pharmaceutical interventions (NPIs)
The researchers also found that lockdown timing was a key factor in determining the final size of the epidemic in England. If it had been a week earlier, the deaths from the first wave might have been as low 15,700 rather than 36,700. If a week later, the deaths might have increased to 102,600, according to this model. The phase of the epidemic in various regions affects the impact of the lockdown. “Initiating a lockdown to interrupt the exponential growth phase of an epidemic has a much greater impact on reducing total mortality than extending an existing lockdown.”
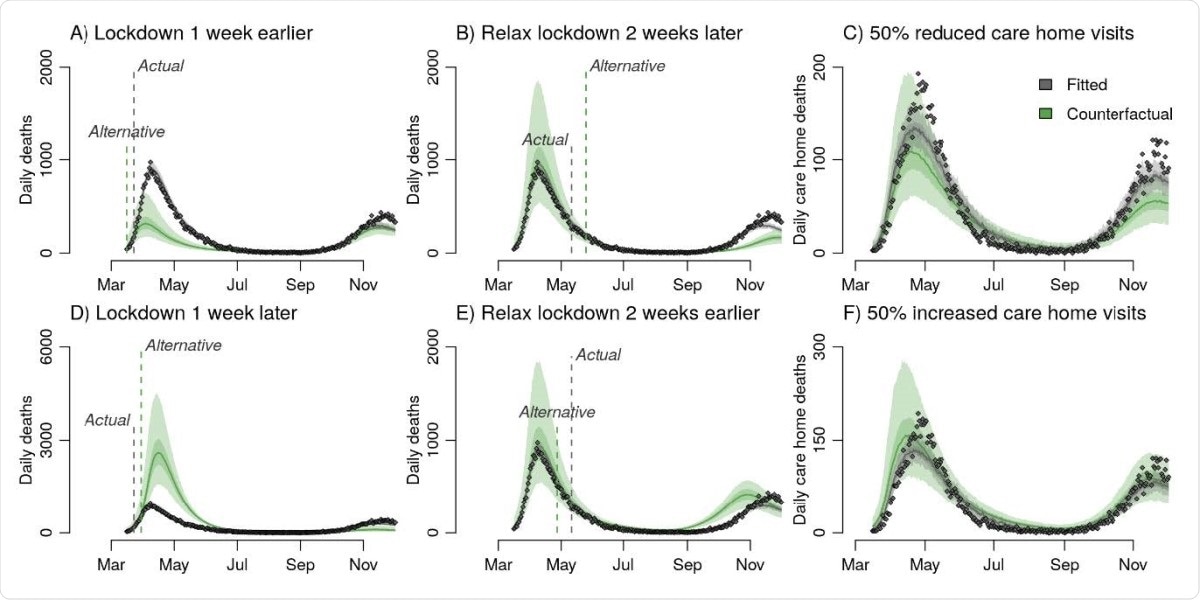
Counterfactual analysis of the impact on mortality aggregated across NHS England regions of A, D, initiating lockdown one week earlier / later, B, E Relaxing lockdown two weeks earlier / later, and C, F 50% more / less restricted care home visits. Panels A, B, D and E all present counterfactual outcomes for daily deaths in England but have different y axis scales to better highlight differences between the observed data and each alternative lockdown scenario.
if the level of visits to care homes had been reduced by half, almost 45% of deaths in these facilities could have been restricted.
What are the implications?
After completing a comprehensive overview of the outbreak across the country, the researchers found that care homes experienced intensive spread during the first lockdown, despite the Reff dipping below 1 in all other areas. This shows the difficulty of infection control in this setting, where there is close contact between the caretakers and other staff, and the residents. Moreover, any outbreak within a home is difficult to contain, even if the number of visitors is restricted.
The observed reduction in the IFR by twofold is not only due to dexamethasone, but because of factors such as better management, greater experience with the pandemic, and expansion of capacity to care for COVID-19 patients. Regional variations in the disease burden were also significant, and may reflect the phase of the outbreak in each area when the lockdown was imposed.
The take-home lesson, however, is that interventions must be implemented early in order to reduce the final mortality. As vaccination campaigns begin, current population immunity estimates are low, from ~5% to ~15%, making high coverage with an effective vaccine an essential requirement for any semblance of return to normal life. Special attention should be paid to care home residents to avoid a return of high mortality rates in this setting.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Knock, E. S. et al. (2021). The 2020 SARS-CoV-2 epidemic in England: key epidemiological drivers and impact of interventions. medRxiv preprint. doi: https://doi.org/10.1101/2021.01.11.21249564,https://www.medrxiv.org/content/10.1101/2021.01.11.21249564v1
- Peer reviewed and published scientific report.
Knock, Edward S., Lilith K. Whittles, John A. Lees, Pablo N. Perez-Guzman, Robert Verity, Richard G. FitzJohn, Katy A. M. Gaythorpe, et al. 2021. “Key Epidemiological Drivers and Impact of Interventions in the 2020 SARS-CoV-2 Epidemic in England.” Science Translational Medicine 13 (602). https://doi.org/10.1126/scitranslmed.abg4262. https://www.science.org/doi/10.1126/scitranslmed.abg4262.