Among the many complications that have emerged from coronavirus disease 2019 (COVID-19), cardiovascular events have become prominent.
The researchers recently published their findings in the Journal of Thrombosis and Thrombolysis.
Study details
The study took a retrospective observational cohort design. It included over 400 subjects enrolled in the COVID-19 Registry to Assess Frequency, Management, and Outcomes of Arterial and Venous Thromboembolic Complications (CORONA-VTE).
All data came from electronic health records from hospitals in the Massachusetts General Brigham healthcare network. The subjects were followed up for 30 days, and the patient outcomes were assessed by a three-person panel.
The outcomes examined were the conventional cardiovascular events; namely, major adverse cardiovascular events (MACE), major arterial and venous thrombosis, and all-cause mortality. MACE was a composite score including venous thromboembolism, myocardial infarction, ischemic stroke, transient ischemic attack, systemic embolism, major adverse limb events, heart failure hospitalization, new atrial fibrillation, and myocarditis.
Several variables were assessed for their potential effect on clinical outcomes. These included age, race, sex, smoking status, body mass index, rhesus (Rh) status, pre-existing atherosclerosis, heart failure, atrial fibrillation, history of chronic anticoagulant or antiplatelet use, and statin therapy.
Blood group association with outcomes
When classified by blood group, about half had blood group O, while about 30%, 15% and 6% had blood type A, B and AB, respectively. People who had a history of cerebrovascular events, who were non-Hispanic whites, or smokers, had a greater chance of having blood group A than O. Hypertensive patients were less likely to have blood group B than O.
Blood groups A and AB were associated with the highest incidence of all three major outcomes. However, when other variables were adjusted for, the odds of MACE were 2.5 times more common in blood group A than blood group O. A strong trend was observed for an increased risk of major thromboses in blood group A as well, at twice the frequency of blood group O, but this did not reach statistical significance. Again, mortality from all causes failed to show any relationship with the blood group.
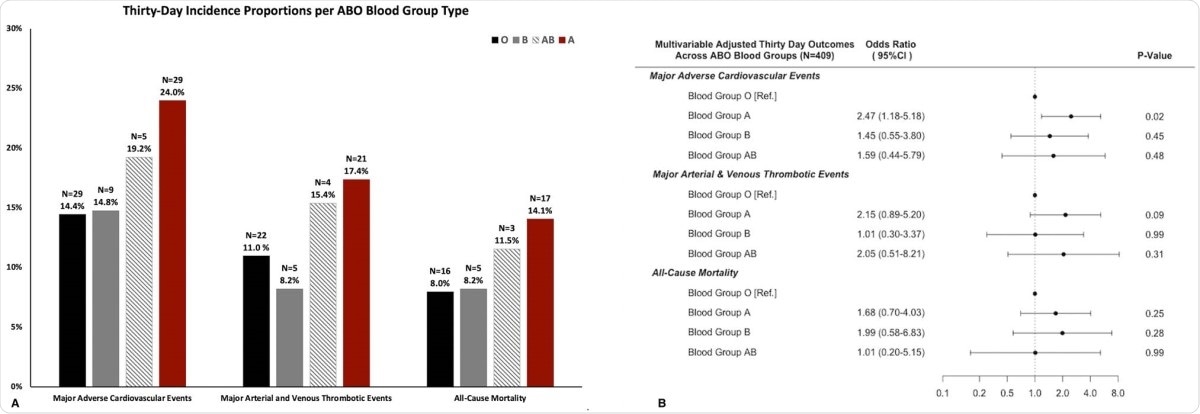
a 30-day unadjusted incidence proportions of major adverse cardiovascular events, major thrombotic events and all-cause mortality per ABO blood group type (N represents absolute number of events). b Forest plot of multivariable association of ABO blood group type with thirty-day major adverse cardiovascular events, major thrombotic events and all-cause mortality. The multivariable model is adjusted for age, race, sex, cigarette smoking status, body mass index, rhesus antigen status, established atherosclerotic cardiovascular disease, heart failure, atrial fibrillation, chronic therapeutic anticoagulation, chronic antiplatelet therapy and statin therapy.
Compared with all other blood groups, blood group A showed over twofold higher odds of MACE, and blood group O had only half the odds. Thus, blood group A had twice the odds of MACE. This adds to the findings of an earlier genome-wide association study that showed an association between the ABO locus and a higher chance of respiratory failure in COVID-19. In that recent study, it was shown that blood group A has a higher risk of respiratory failure in this infection, and blood group O a reduced risk.
What are the implications?
The current study indicates that the ABO gene locus is associated with cardiovascular complications in patients with COVID-19. Some studies show that natural antibodies to glycan ABO antigens inhibit the SARS-CoV’s entry into the host cell, via the interaction between the viral spike glycoprotein and the angiotensin-converting enzyme 2 (ACE2) receptor.
Blood groups other than O have also been found to associate with higher frequency of both arterial and venous clots, perhaps because they have higher levels of von Willebrand factor and factor VIII – both potent clotting factors.
The researchers point out that this association cannot be taken to prove a causal role for the ABO blood group types in the pathogenesis of cardiovascular complications in COVID-19, and that further study is required.
They call for larger and more long-term studies to confirm these associations. At the current level of knowledge, these findings may help identify patients who are possibly at greater risk for these adverse outcomes, in order to provide optimal management and care.