A study recently published in the journal Cureus has described a case report of a coronavirus disease 2019 (COVID-19) patient who presented with pneumonia, posterior reversible encephalopathy syndrome (PRES), and persistent cortical blindness. A detailed clinical presentation of the patient is provided in the report.
Background
Since the emergence of the COVID-19 pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), several studies have been done to identify the specific signs and symptoms as well as adverse complications associated with the disease. Besides pulmonary and cardiovascular adversities, severe COVID-19 patients have been found to present with neurological complications, including headache, dizziness, encephalopathy, delirium, meningitis, encephalitis, acute transverse myelitis, and smell and taste disorders. In this context, studies have shown that COVID-19 associated neurological complications are primarily caused by direct viral invasion and inflammation in the neuronal network.
In the current case report, the scientists have described the clinical consequences of a 54-year-old COVID-19 patient who presented with SARS-CoV-2 related pneumonia, posterior reversible encephalopathy syndrome (PRES), and persistent cortical blindness.
Important observations
The patient's initial clinical presentations were fever, dry cough, and myalgia for ten days, in addition to significant breathlessness. At the time of hospital admission, the patient had a high body temperature, significantly elevated heart rate, and 82% oxygen saturation level. Because of further deterioration of the health condition of the patient, non-invasive ventilation was started.
According to the clinical examinations, the patient had lower levels of lymphocytes in the blood; however, no abnormalities in renal function, electrolyte balance, and blood coagulation profile were observed. Based on the chest x-ray observation of bi-basal consolidation and a SARS-CoV-2 positive respiratory swab sample, the patient was empirically administered with amoxicillin/clavulanic acid and clarithromycin.
Because of increased oxygen demand, the patient was subjected to endotracheal intubation and mechanical ventilation after ten days of admission. With further examinations, the patient was diagnosed with acute respiratory distress syndrome and systemic inflammatory response syndrome. Based on the patient's clinical profile, a possibility of sepsis could not be ruled out, and thus, the treatment with broad-spectrum antibiotics was initiated. Throughout the course of the hospital stay, the patient was not administered any steroids or immunomodulatory medicines.
On day 21, the patient had a generalized seizure and a brain CT scan was performed, which suggested the possibility of PRES. Although the patient gradually became stabilized and the mechanical ventilation was removed, neurological examination demonstrated the presence of complete cortical blindness and Anton's syndrome (denial of loss of vision). Although the patient started recognizing shapes and colors because of gradual physical and neurological recovery, a significant level of visual impairment persisted.
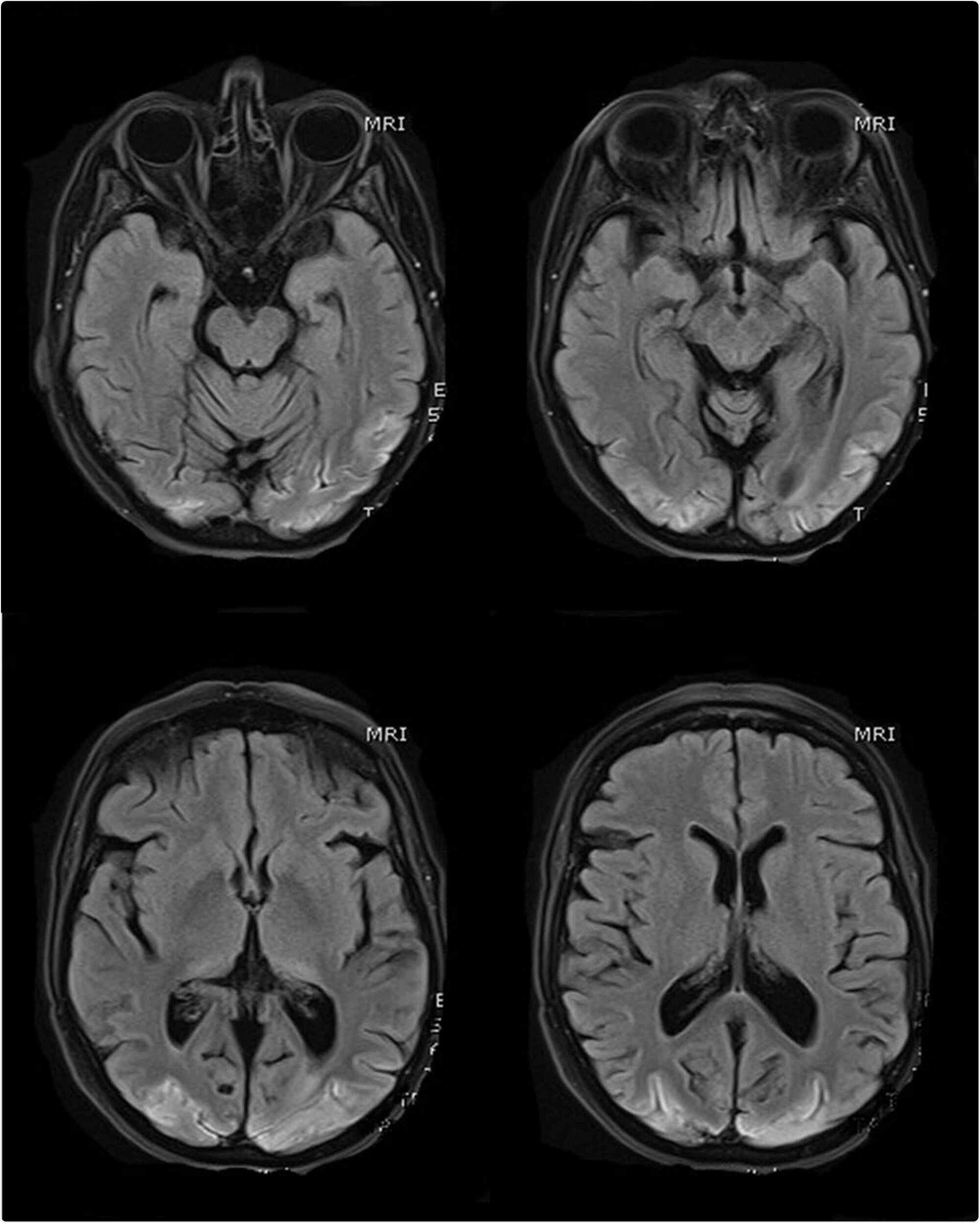
MR scans of the brain (selected T1 sequences) show bilateral symmetrical hyper-intensity involving the bilateral occipital lobe cortex; the changes are consistent with cortical pseudo-laminar necrosis as a complication of posterior reversible encephalopathy syndrome (PRES)
The significance
According to the available literature, cerebral hyper-perfusion caused by hypertension is a significant risk factor for PRES. Thus, the authors suggest that tight regulation of blood pressure is essential for COVID-19 patients to avoid the risk of PRES, which is otherwise a rarely observed SARS-CoV-2-related complication. However, in the current study, the patient's highest blood pressure was 190/90 mmHg just after the first seizure. Otherwise, the patient displayed normal blood pressure throughout the hospital stay. Therefore, the authors suggest that high blood pressure is not the primary reason for PRES in this case.
Because sepsis was suspected, the authors suggest that COVID-19-related endothelial dysfunction might be a potential cause of PRES.
Taken together, the authors suggest that PRES, along with persistent cortical blindness, should be regarded as one of the rare complications associated with SARS-CoV-2 infection.
Source