The coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused immense loss of life and health, as well as economic and psychological well-being. While most infections with the virus are asymptomatic or cause only mild disease, a significant minority of patients develop severe respiratory distress requiring mechanical ventilation, often leading to death, either directly or in association with multisystem failure.
In the absence of specific antivirals to combat the pandemic, supportive care is paramount. In this context, a new preprint posted to the medRxiv* server describes the observed efficacy of prone positioning to reduce mortality and the risk of intubation in COVID-19 patients with respiratory insufficiency.
Prone positioning
Prone positioning (PP) is no new thing, having been demonstrated about 45 years ago to result in higher oxygenation in patients with respiratory insufficiency.
In patients with acute hypoxemic respiratory failure, but are not intubated, placement in the prone position (PP) is associated with an increase in the arterial partial pressure of oxygen (PaO2), peripheral arterial oxygen saturation (SpO2), and PaO2/inspired oxygen fraction (PaO2/FiO2). This indicates improved oxygenation.
At the same time, there are no adverse effects on the level of partial arterial pressure of carbon dioxide (PaCO2), pH, respiratory rate (RR), or on the circulation as a whole. Thus, PP in combination with non-invasive ventilation (NIV) or high-flow nasal cannula (HFNC) has been established as both effective and safe in patients with acute respiratory distress syndrome (ARDS) of moderate to severe degree.
The mechanisms operating in the PP may include enhancing the functional residual capacity, which refers to the lung volume filled with air after a maximal exhalation; reducing the dead space, or lung volume where gas exchange is not occurring; reducing arteriovenous shunts within the lung; increasing ventilation in lung areas that are dependent; and preventing the weight of the heart from impinging on the inflamed lungs.
These benefits have led to a spurt in scientific interest in and application of PP in awake non-intubated patients. In fact, in such severe COVID-19 cases, combinations of PP+NIV or PP+HFNC have been shown to reduce the intubation and mortality rates while enhancing the patient's oxygenation status.
Another important advantage is that PP avoids intubation and allows the sick individual to interact with family members during this need. This introduces a much-needed human element into medical care.
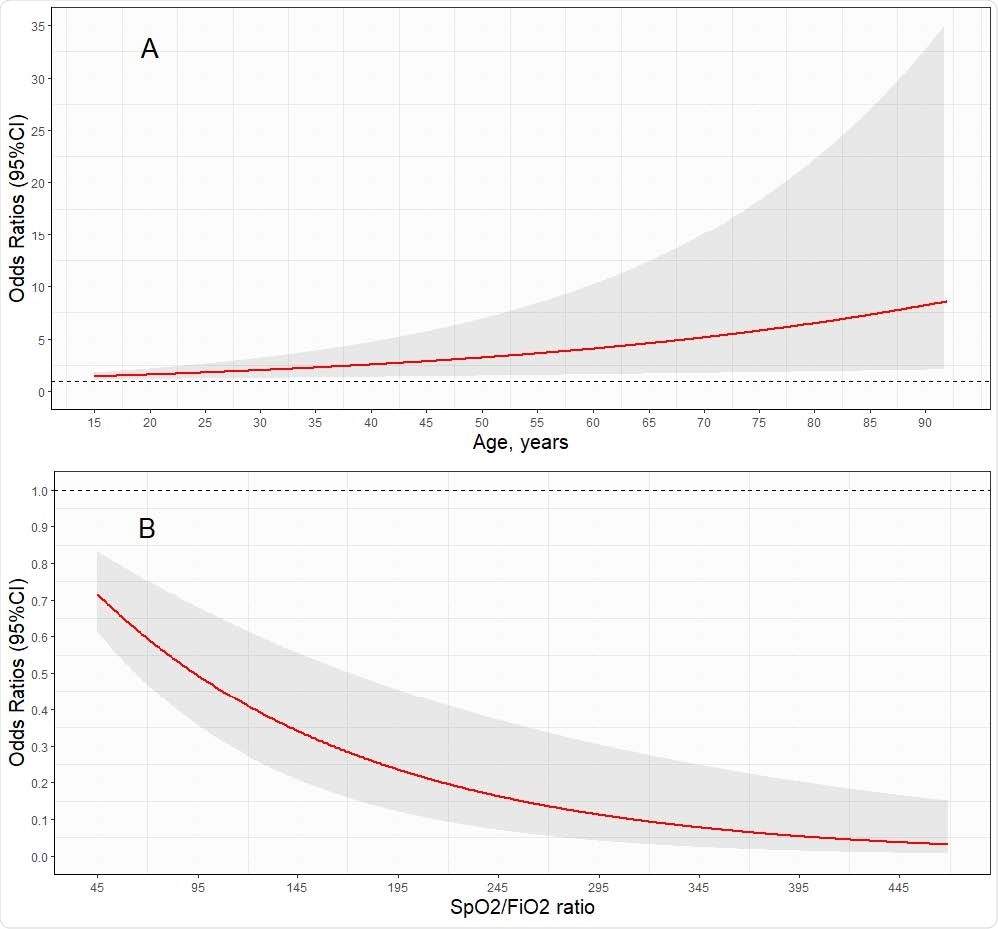
Risk of prone positioning failure according to age and baseline SpO2/FiO2

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Disadvantages of supine position
When a patient with respiratory difficulty is in the supine position, the dependent and non-dependent areas of the lung experience differences in the gravitational forces acting on them. This causes a change in lung function.
For instance, the pleural pressure becomes negative, and the transpulmonary pressure (TPP) becomes higher in the non-dependent areas. The opposite changes occur in the dependent regions.
Ventilation in the PP allows a uniform TPP, which favors the ventilation-perfusion ratio. This is the primary reason for the well-established improvement in oxygenation with PP in patients with respiratory insufficiency.
Study aims
Some observational studies comparing patients on PP with those on NIV or HFNC, have produced discordant findings. The current multicenter observational study aimed to develop a model that would predict the outcome of PP in awake patients, with respect to the need for intubation, and to contribute to an understanding of the relationship between awake PP and mortality.
Study details
The study included 827 patients, over 27 centers. Of the original 932 patient cohorts, 27% were female and the average age was 54 years. The majority of patients were 50-59 years old. The mean age is less than that in other studies.
Almost 40% and 35% of patients had diabetes and hypertension. The overall prevalence of coexisting illness is similar to that in earlier studies, though the prevalence of diabetes is higher. Obesity and heart disease are less common.
Half the patients were successfully managed with low-flow nasal cannulas. Patients were individually assigned in a non-random fashion to the awake supine or awake prone position (AS and AP groups, respectively).
Multiple variables were incorporated into the model to find the risk of subsequent intubation, indicating PP's failure. The results were used to construct the final classification and regression tree (CART) model.
PP associated with reduced intubation risk
The researchers observed that while 40% of AS patients required eventual intubation, only 24% in the AP group did. The SpO2/FiO2 ratio in the latter was markedly higher relative to the baseline 217 and 182, respectively.
The risk factors for failure of PP and switch to orotracheal intubation included advanced age, diabetes, hypertension, obesity, cancer, heart disease, as well as SpO2/FiO2 <100 at baseline, or 100-199 at any point, and if a non-rebreather mask is used.
After adjusting for multiple confounding factors, SpO2/FiO2 <100 at baseline increased the risk by 178%, while a value between 100 and 199 increased it by 218%. The use of a non-rebreather mask similarly increased the risk by 217%.
However, the use of ventilation in the AP group was protective against intubation and mortality. The overall mortality was 20%, which is similar to that reported in earlier studies.
CART predictions
The researchers predicted, from the CART model, that an initial or admission SpO2/FiO2 ratio <177.6 is linked to a higher risk of intubation. In this case, the risk of intubation is 43.5%, but below this, the risk is only 16%. Again, in the first group, the use of PP is credited with reducing the risk of intubation from 66.4% to 30.8%.
An earlier study found that patients with SpO2 at 95% or greater, and those with less than this value, had a difference of 46% in the rates of intubation.
What are the implications?
The study suggests that awake PP is associated with a lower risk of intubation and mortality in hospitalized COVID-19 patients. The only medical conditions that were linked to a higher risk of intubation after adjusting for confounding factors were diabetes and heart disease. Even so, the propensity score analysis removed diabetes from the list of risk factors.
A high baseline SpO2/FiO2 was linked to a reduced risk of intubation. In older patients, the risk of PP failure was higher in an age-dependent fashion.
The researchers point to PP's utility in avoiding mechanical ventilation in patients with COVID-19 and respiratory distress, especially in low-resource countries.
The CART model could provide vital information to aid in decision-making as to the need for PP in a patient, irrespective of the type of oxygenation device used in such settings.
There were necessarily variations in the number of hours spent in the PP, the type of oxygenation devices, and intubation criteria since a large number of centers participated in the study. However, this is also valuable since it mirrors PP's actual use in the real clinical setting.
This remains the most extensive study exploring AP's role and underlines the benefits of PP to the awake non-intubated patient, whether or not NIV or HFNC devices are also used. Further validation should be sought through randomized controlled trials since this is an inexpensive, easily applied and reproducible modality of intervention with an excellent safety profile.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Awake prone positioning and oxygen therapy in patients with COVID-19: The APRONOX study Orlando R. Perez-Nieto, Diego Escarraman-Martinez, Manuel A. Guerrero-Gutierrez, Eder I. Zamarron-Lopez, Javier Mancilla-Galindo, Ashuin Kammar-García, Miguel A. Martinez-Camacho, Ernesto Deloya-Tomás, Jesús S. Sanchez-Diaz, Luis A. Macías-García, Raúl Soriano-Orozco, Gabriel Cruz-Sánchez, José D. Salmeron-Gonzalez, Marco A. Toledo-Rivera, Ivette Mata-Maqueda, Luis A. Morgado-Villaseñor, Jenner J. Martinez-Mazariegos, Raymundo Flores Ramirez, Josue L. Medina-Estrada, Silvio A. ñamendys-Silva medRxiv 2021.01.27.21250631; doi: https://doi.org/10.1101/2021.01.27.21250631, https://www.medrxiv.org/content/10.1101/2021.01.27.21250631v1
- Peer reviewed and published scientific report.
Perez-Nieto, Orlando R., Diego Escarraman-Martinez, Manuel A. Guerrero-Gutierrez, Eder I. Zamarron-Lopez, Javier Mancilla-Galindo, Ashuin Kammar-García, Miguel A. Martinez-Camacho, et al. 2021. “Awake Prone Positioning and Oxygen Therapy in Patients with COVID-19: The APRONOX Study.” European Respiratory Journal 59 (2): 2100265. https://doi.org/10.1183/13993003.00265-2021. https://erj.ersjournals.com/content/59/2/2100265.