The blood-brain barrier prevents immune cells from circulating freely in the brain, and the breakdown of its function is a major cause of post-stroke inflammation. Now, for the first time, researchers have identified how a toxic stroke byproduct, acrolein, could activate the barrier-degrading enzyme proheparanase (proHPSE). The research group has discovered that proHPSE degrades the glycocalyx within the post-stroke brain's blood vessels, providing hope for new and effective therapeutics against post-stroke inflammation.
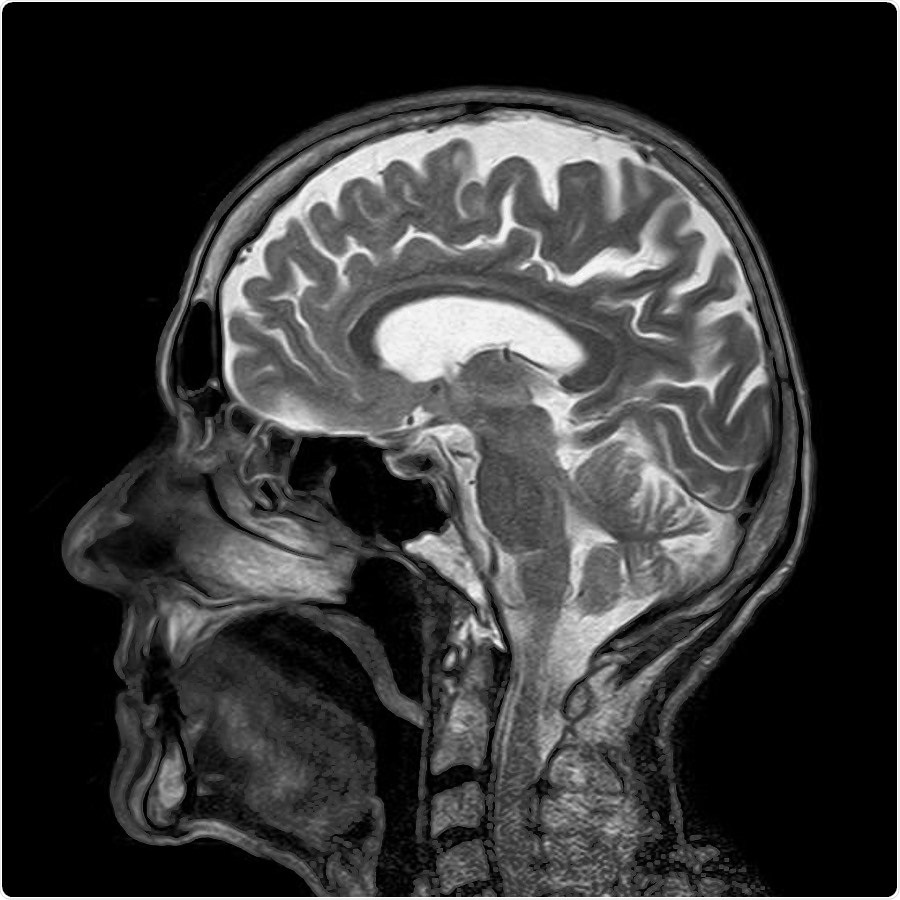
Image Credit: Tokyo University of Science
Strokes are a leading cause of poor quality of life or even death in Japan and the world over. Since its characterization, several researchers have been working tooth and nail to identify drug-accessible and effective therapeutic targets for this debilitating condition. One such region of interest for drug targets is the blood-brain barrier (BBB).
The BBB is a structure located around the brain, which prevents the entry of unnecessary circulating cells and biomolecules into the brain. The blood vessels in the BBB are coated with a distinct and protective layer of sugar, called the endothelial glycocalyx, which prevents their entry.
However, in the event of a stroke, which results in the blockage or severance of blood vessels in the brain, studies have shown that this glycocalyx and, in turn, the integrity of the BBB, get compromised. In addition, damage to the blood vessels leads to neuronal death and the build-up of toxic byproducts like acrolein.
A group of researchers from Japan and the United States wanted to explore how the degradation of the glycocalyx takes place during an ischemic stroke.
When brain tissue becomes necrotic due to ischemia, the function of the BBB is disrupted and immune cells infiltrate the brain, exacerbating inflammation, but the details of this process are still unclear."
Kyohei Higashi, Junior Associate Professor, Tokyo University of Science
For the first time, as detailed by the study published in Journal of Biological Chemistry, the group of scientists, led by Dr. Higashi, have identified a possible mechanism that links acrolein accumulation to glycocalyx modifications, which results in damage to the BBB.
The team, also comprising Naoshi Dohmae and Takehiro Suzuki from RIKEN Center for Sustainable Resource Science, Toshihiko Toida from Chiba University, Kazuei Igarashi from Amine Pharma Research Institute, Robert J. Linhardt from Rensselaer Polytechnic Institute, and Tomomi Furihata from Tokyo University of Pharmacy and Life Sciences, used mouse models of stroke as well as in vitro ("in the lab") experiments using cerebral capillary endothelial cells to accurately study the mechanisms behind the breakdown of the BBB.
The researchers initially identified that the major sugars in the glycocalyx, heparan sulphate and chondroitin sulfate, showed decreased levels in the 'hyperacute phase' after a stroke. They also found the increased activity of glycocalyx-degrading enzymes like hyaluronidase 1 and heparanase. Upon further in vitro investigation using cell lines, they found that acrolein exposure led to the activation of the precursor of heparanase (proHPSE).
Specifically, they found that the acrolein modified specific amino acids on the structure of proHPSE, activating it. They concluded that this mechanism possibly led to the degradation of the glycocalyx, and the subsequent disruption of the BBB.
The team's discovery is critical, as the acrolein-modified proHPSE could be a novel and potentially effective drug target for post-stroke inflammation. As Dr. Higashi, who is also the corresponding author of the study, speculates, "Because proHPSE, but not HPSE, localizes outside cells by binding with heparan sulfate proteoglycans, acrolein-modified proHPSE represents a promising target to protect the endothelial glycocalyx."
Indeed, we hope that the further investigation of this mechanism would lead us to therapies that are more effective in tackling stroke-related illnesses!
Source:
Journal reference:
Ko, K., et al. (2020) Ischemic stroke disrupts the endothelial glycocalyx through activation of proHPSE via acrolein exposure. Journal of Biological Chemistry. doi.org/10.1074/jbc.RA120.015105.