Vaccination against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has rolled out in many countries, including the United States. As the number of coronavirus disease (COVID-19) cases continues to rise, vaccinating many people in the population is crucial. Despite campaigns to inform residents of the benefits of vaccines, many are still reluctant to get vaccinated.
Researchers at the Massachusetts General Hospital, the Johns Hopkins Hospital, and the University of California, San Francisco, found that over one-third of the study respondents were hesitant to get the COVID-19 vaccine. To increase vaccine acceptance, the team suggested public health interventions to target vaccine-hesitant populations, with messaging that addresses their concerns about the vaccines' efficacy and safety.
COVID-19 vaccination
There are more than 250 vaccines against COVID-19 in development by pharmaceutical companies across the globe. Of these, 71 are in clinical evaluation. Vaccines are now being widely administered, these include Moderna's vaccine, the Pfizer+BioNTech vaccine, the AstraZeneca + University of Oxford vaccine, and more recently the Johnson & Johnson vaccine.
One of the ways to combat the COVID-19 pandemic is attaining herd immunity. For COVID-19 vaccination to effectively confer herd immunity, health experts said that at least 60 to 70 percent of the population must be vaccinated.
However, vaccine hesitancy deters this. For instance, influenza vaccine hesitancy rates have increased by about 40 percent. The researchers aimed to see the most common reasons why Americans are hesitant to get vaccinated for COVID-19.
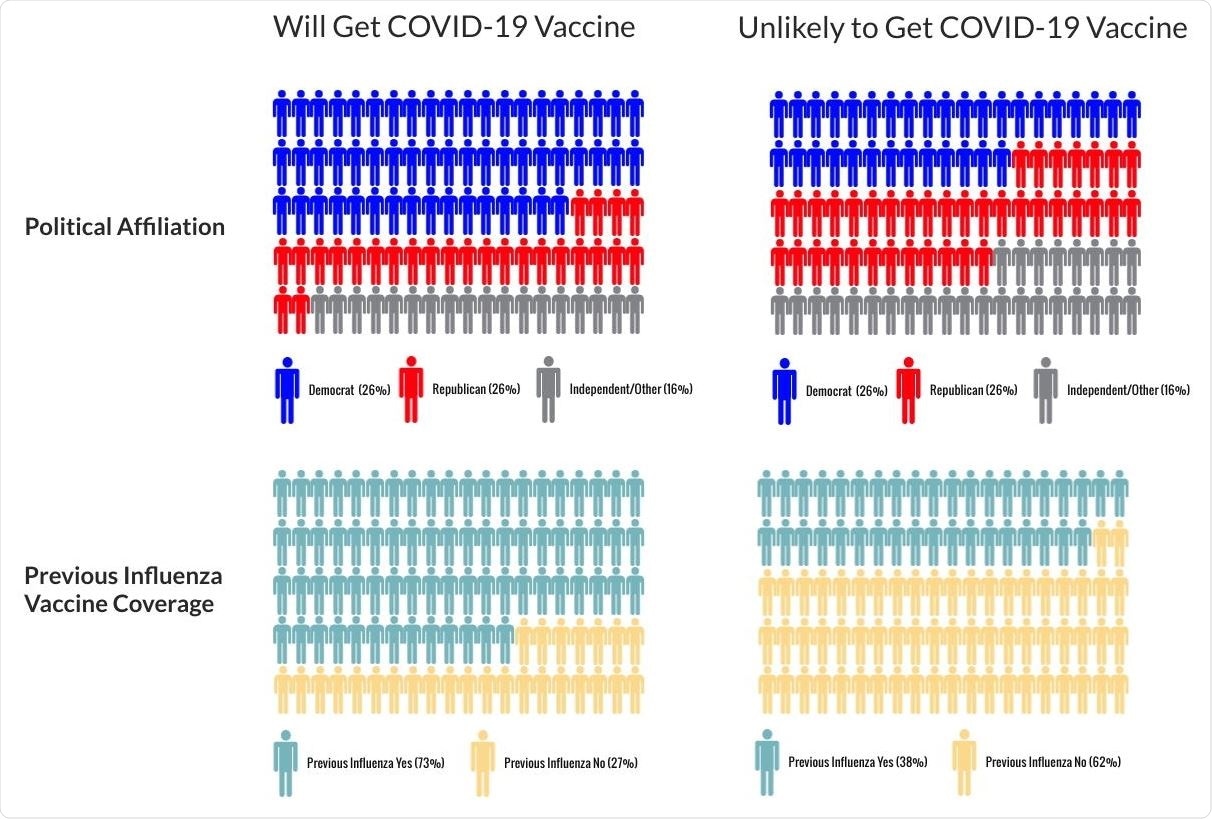
Main Predictors of Covid-19 Vaccine Hesitancy Personograph plot of the classification tree analysis, which identified previous influenza vaccine coverage and political affiliation as significant predictors of COVID-19 vaccine hesitancy. The main reasons given for vaccine were concerns about side effects and safety of the vaccine (75%, n=497), the need for more information about the vaccine (53%, n=351), and doubts regarding the efficacy of the vaccine (17%, n=110).

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
The study
The study, published on the preprint server medRxiv*, aimed to determine the U.S. population rate of COVID-19 hesitancy, identify characteristics linked to hesitation, and determine the reasons for reluctance.
The researchers distributed a 43-question survey on Amazon Mechanical Turk, an online labor marketplace where people receive a nominal fee for completing tasks, to 1,756 respondents between November 17 and 18, 2020.
The expected primary outcome measure was the rate of COVID-19 vaccine hesitancy, which is defined as either non-acceptance or being unsure about accepting the vaccine. Secondary outcomes included patient characteristics tied to vaccine hesitancy, reasons for being hesitant, and health care sites where they would like to be vaccinated.
Study findings demonstrated that a total of 663 participants were COVID-19 vaccine-hesitant, wherein 374 were decided to be non-acceptors, and 289 were unsure about accepting the vaccine.
Further findings showed that vaccine hesitancy was tied to not receiving the influenza vaccine in the past five years. Also, females, Blacks, having a high school education or less, and being in the Republican party affiliation were more likely to be vaccine-hesitant.
The reasons cited for vaccine hesitancy included the potential side effects, the need for more information about the vaccine, and doubts about vaccine effectiveness. For the preferred cites for vaccination, vaccine acceptors opted to go to their primary doctors, dedicated vaccination areas, and pharmacies.
"Optimal health policy deliberations for COVID-19 vaccine distribution require consideration of vaccine hesitancy and reasons for refusal," the researchers explained.
"To improve efficient and equitable vaccine distribution, educational messaging campaigns should seek to address non-acceptors' primary concerns of safety and side effects of the vaccine," they added.
The team also recommended widening the efforts to disseminate information on the benefits of vaccination against infections. This can help control and spread the virus, and at the same time, aid in the attainment of herd immunity.
As the virus continues to wreak havoc globally, boosting vaccination campaigns can help control the pandemic. To date, more than 115 million people have already been infected with SARS-CoV-2. Of these, 2.55 million have died.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Source:
Journal reference:
- Preliminary scientific report.
Raja, A., Niforatos, J., Anaya, N., Graterol, J., and Rodriquez, R. (2021). Vaccine hesitancy and reasons for refusing the COVID-19 vaccination among the U.S. public: A cross-sectional survey, medRxiv. https://doi.org/10.1101/2021.02.28.21252610, https://www.medrxiv.org/content/10.1101/2021.02.28.21252610v1