I have been working on head and neck cancer for 30-40 years and one of the things that has driven me is to try and reduce the magnitude of surgeries. You can imagine how destructive treatment can be to mouths, jaws, and the face.
Small blemishes that can be easily hidden on, for example, the bowel or belly have a huge impact on patient form and function when in the face. I have been slowly moving away from major surgeries and instead of looking for minimally invasive surgeries that produce the same, if not better outcomes.
We have developed several different techniques to minimize the magnitude of surgery, we have introduced Sentinel Node Biopsy(SNB) to the UK, we now have methods of stopping jaws from being removed for odontogenic tumors and this particular treatment is a huge advancement in treatment for salivary glands.
I have had a real interest in salivary glands and two or three things have come together in the last year to create this new treatment. I have a brilliant radiologist called Simon Morley who has found a way of tracing the facial nerve, and by putting this together with some new technology we have been able to make a huge breakthrough.
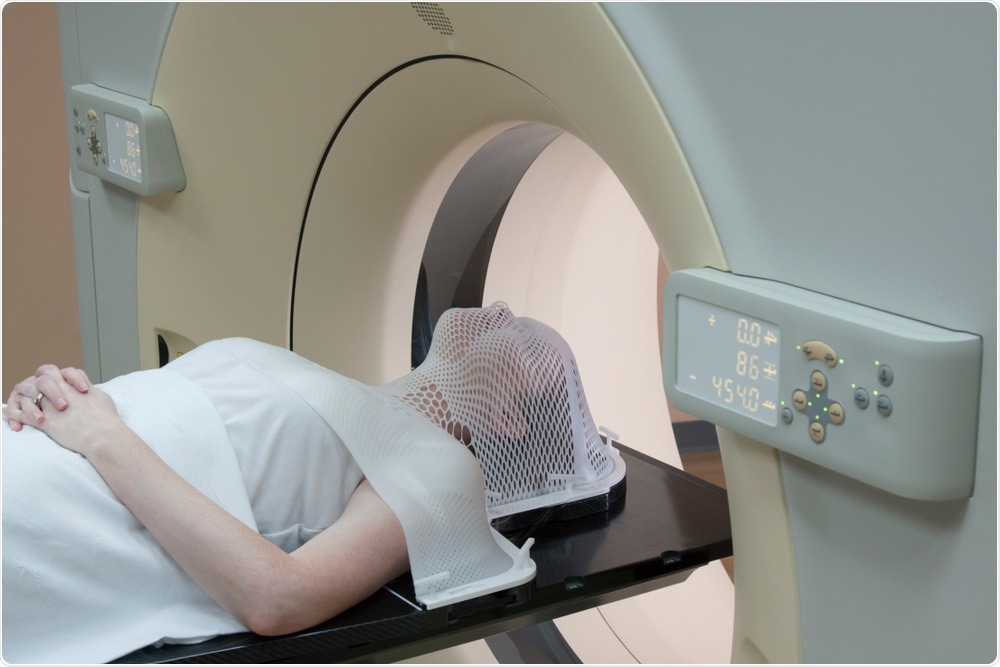
Scan for Head and Neck Cancer. Image Credit: Mark_Kostich/Shutterstock.com
Your latest research investigated salivary gland tumors. Why do over three-quarters of salivary gland tumors start in the parotid gland?
The parotid gland is the biggest salivary gland, so this is purely a reflection of size. The more glandular tissue in an area the more chance there is of something going wrong.
Why is surgery difficult when faced with these types of tumors?
Surgery is difficult because the parotid gland sits on the side of your face and the facial nerve comes out from deep in your skull and passes through the gland before breaking into smaller branches to cover the face. This is a small nerve; the main trunk of the nerve is only about 1mm in diameter.
However, it is vital to controlling your face, which allows you to convey emotion. Therefore, damage to this nerve has a great impact on a person’s form and function. Historically, this has become a dominant-negative effect from head and neck cancer treatment. Because it runs through the gland, it is easy to hit and damage the nerve during surgery.
The traditional approach was very maximal, it required surgeons to open up the face and locate the nerve during surgery. Surgeons have to carefully lift the tissue above the gland to access the top of the gland. Most of the gland is found above the nerve, meaning that the majority of tumors are located in the top section.
When the tumor is located in the top section, this is called a superficial parotidectomy. If the tumor is below the nerve, the surgeon will have to carefully tease the nerve off of the gland this is called a total parotidectomy with preservation of the nerve. As you can imagine, these operations have a high risk of damage. A total parotidectomy carries a 60% incidence of temporary nerve injury and a 4-6% incidence of permanent damage. Superficial parotidectomies carry a 30% rate of temporary damage and a 1% rate of permanent damage.
This operation is specifically difficult as you don’t know where the nerve is or what the tumor has done to the nerve, making surgeons more or less blind when going in. This technique has stood the test of time, it was introduced in the 1940’s/50’s. Surgery has now moved on but has left parotid surgery behind.
Can you describe your research that has led to the groundbreaking new procedure for salivary gland tumors? How does this procedure work?
There have been developments in MRI scanning, the machines essentially use much bigger magnets now which allow the scans to produce more detail, with each layer being less than a millimeter apart. This allows us to now find the tiny nerves that come out of the skull base, these can be followed through the gland, though still difficult. Our radiologist picked up on this quicker than most and began to draw diagrams of this.
The initial diagrams were hard to understand and did not represent the 3d dimensions. It just so happened that I was working with the Microsoft HoloLens, which produces augmented reality holograms, for other purposes. We looked into whether we can take the information from the MRI scan, along with Simon’s tracings of the nerve, and turn these into holograms.
We are currently the only team in the world who can do this, although we have been trying very hard to export this to a number of units in the far east, USA, and throughout Europe.
The advantage of this is that we now have a more minimal approach that works with this treatment, which came from a team in Manchester years ago. This involves peeling back a smaller part of the skin and carefully dissecting the lump, almost opening it up like a flower in the sense of peeling back each petal. This still meant that surgeons were working blind meaning that they were reluctant to pick up the procedure even though it statistically much better results in terms of injury and morbidity.
The fact that we have this new visual information coming in and a technique that can accommodate this allows us to reduce the size of the operation and move to a minimally invasive approach, as many surgeries have done or are heading towards.

Salivary Gland Tumor. Image Credit: Orawan Pattarawimonchai/Shutterstock.com
Do you believe that this procedure will help to plan more accurate surgeries and improve patient outcomes? Why is this?
Yes, I do. There is still a lot of new developments coming in. Currently, you can look at the hologram of the gland, interact with it and examine it before surgery. We are now only a few months away from having the hologram co-localized onto the patient during surgery. This allows us to essentially see through patients and plan exactly where to make cuts.
I think this will facilitate the introduction of more minimally invasive surgery, improve it, and make it more reliable.
What are some of the limitations and barriers with this treatment option?
Right now, you have to have an enthusiastic radiologist as it can be a lot of extra work, each model can take 40 minutes to build. The radiologist also has to have a good eye to track the nerve. We can get over this by using artificial intelligence and machine learning to assist with tracing the larger structures such as the parotid gland and jaw, this is a few years away.
The cost of the equipment is not that expensive, it is really the extra work put on to the radiologist. I think surgeons may be reluctant to change and embrace new technologies, and it may be the younger surgeons that take this on more. However, these are not large limitations to us.
As more advanced technology and software becomes available, do you believe that this procedure will continue to become more accurate and precise at detailing the surgery area?
We are only at the start of a revolution in imaging. With new MRI scans, we can see more than ever, you will soon be able to look at a body and see within it using augmented reality. There are a few barriers to this such as breasts and bowels, which are very mobile and will move when a patient goes from lying down to sitting up.
We will likely be able to get over this by using ultrasound to marry into these images and recorrect them in real-time. I envision much more minimally invasive surgeries in the future with this improved imagery and the introduction of things like artificial intelligence. This is just the start.

MRI Scans. Image Credit: sfam_photo/Shutterstock.com
What are the next steps in your research into oral cancer?
Moving forward on a broad front. We have introduced SNB which allows people with early stages of mouth cancer to avoid a full neck dissection, about 70%. We are currently training units to implement this. This technique can be used in the parotid and the skin around the head and neck to reduce the magnitude of surgery.
My career is coming slowly to an end now, many of these projects can take 5-12 years to come to fruition. I want to leave a legacy of people looking at and using new technologies to minimize surgery. This is why I set up the Head and Neck Cancer Foundation.
To leave this legacy, we need two approaches: a flexible mind, meaning not getting stuck on the same techniques, and to utilize new technology that might not be designed for medicine but can be adapted to produce some remarkable results when matched with new technologies in medicine.
Where can readers find more information?
Readers can find more information about the Head and Neck Cancer Foundation and the work Mark is pioneering at www.hncf.org.uk.
About Professor Mark McGurk
Professor McGurk is the director of the Head & Neck Academic Centre at University College London Hospital. His clinical practice has centered on head and neck cancer surgery and minimally invasive management of salivary gland disease as have his research themes.
He has championed minimally invasive surgery for benign parotid tumors and obstructive salivary gland disorders. This has revolutionized the treatment of salivary gland disease and it is now no longer necessary to routinely remove salivary glands for benign disease.