The coronavirus disease (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to wreak havoc across the globe.
The extent of the pandemic is still unknown since many of the infections were asymptomatic.
Serology testing provides a paradigm for estimating the number of individuals who have been infected with SARS-CoV-2, including cases undetectable by routine testing.
Traditional statistical methods to estimate antibody response do not incorporate case counts over time, which may be inaccurate.
Now, scientists at Simon Fraser University developed a joint Bayesian model for case counts and serological data, combining sensitivity and specificity.
In the study, which appeared on the pre-print server medRxiv*, the team also modeled the pandemic phases with exponential growth and decay. The model improves upon maximum likelihood estimates by conditioning on more data.
Estimating the number of cases
More than a year into the pandemic, the number of cases continues to rise. However, many cases are unaccounted for. Asymptomatic carriers, those who never develop symptoms, are not routinely tested.
The SARS-CoV-2 infection may be much more widespread than indicated by the number of confirmed cases.
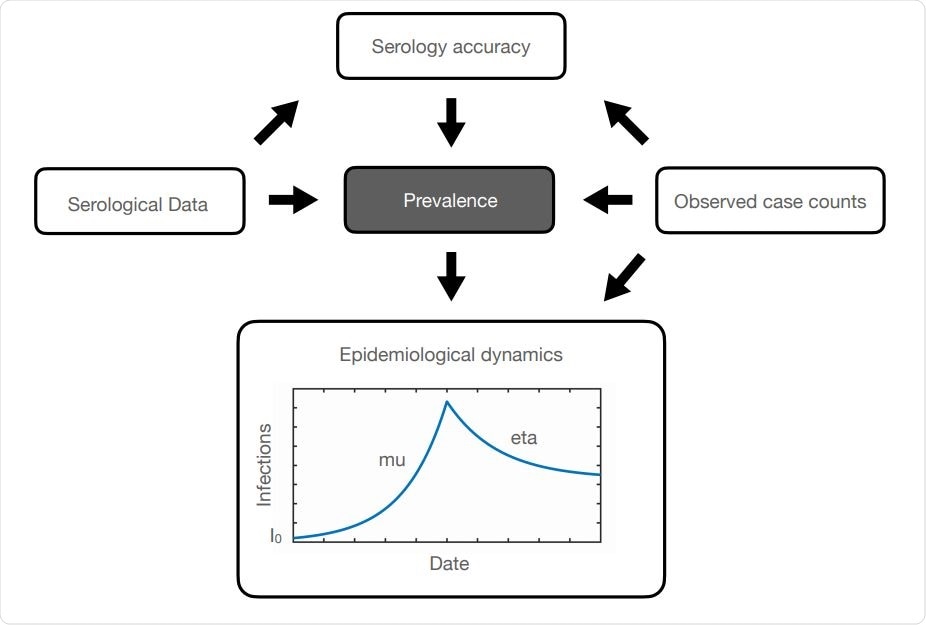
Plate diagram (Koller and Friedman, 2009) indicating the acyclic graph governing the relationships among variables in our model. Arrows indicate conditional dependencies, according to equations in the Methods Section. For epidemiological dynamics, we assume that the number of active cases increases exponentially with rate µ and then decreases according to exponential decay with rate η following the introduction of NPI measures. I0 is the number of initial cases among the population. This schematic represents antibody prevalence during a rise and then a fall of the pandemic over a single Phase. (For example, Phase 1 of the pandemic in B.C. from the end of January until the end of May.)
To know the extent of the COVID-19 pandemic, it is crucial to conduct serology testing. The current study aims to make use of a Bayesian method and apply it to serology and case count data from the greater Vancouver area in British Columbia, Canada, during the first pandemic wave.
The team integrated test sensitivity and specificity with an epidemiological model for case counts to arrive at the study findings. The team improved its method upon previous work in serology measurements by integrating uncertainty about testing accuracy.
The methods allow serological data to be combined with SARS-CoV-2 case counts from polymerase chain reaction (PCR) tests to better estimate the prevalence of antibody response, calculate the number of infections detected, and predict future trends in the coronavirus pandemic.
After computing, the team estimates a posterior mean antibody prevalence of 0.57 percent in the greater Vancouver area during the first pandemic wave. This matches previous estimates of 0.55 percent.
"Our posterior conditions on more data (case counts) and is constrained by disease dynamics, and so we expect less uncertainty in our estimates (this is reflected in our tighter confidence intervals)," the team explained.
The team concluded that the estimates match those from classical methods. However, the group's estimate is more accurate.
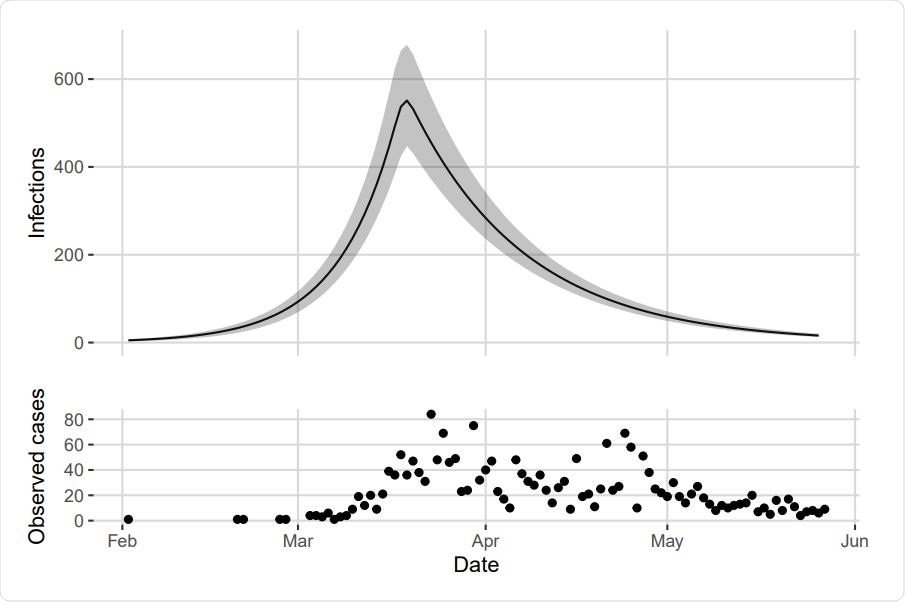
Top: Estimated number of infections in the greater Vancouver area between January 26 and May 27. Posterior mean shown by the solid line with 95% credible band in grey. Bottom: Observed cases in Vancouver over the same time frame.
Importance of serology testing
Antibodies are usually detected in the blood of those tested positive for COVID-19, showing they developed an immune response to the infection. Serology testing determines these antibodies' presence to detect previous infections in those with few or no symptoms.
Apart from detecting the pandemic's extent, serology testing can also help scientists determine how much protection antibodies provide against re-infection. This can also help in current vaccination efforts.
Further, it is designed to estimate the percentage of the population previously infected with the virus. The data can help to guide the response to the pandemic to protect the public's health.
Global case toll
Many countries have imposed new lockdowns as the number of SARS-CoV-2 infections soars. The total number of cases has reached over 127 million, while 2.79 million people have died.
The United States reports the highest number of cases, reaching over 30.33 million, followed by Brazil and India, with over 12.57 million and 12 million, respectively. Meanwhile, France has reported surging cases, with its case toll topping 4.61 million, followed by Russia and the United Kingdom, with 4.47 million and 4.35 million cases, respectively.
Vaccine efforts have rolled out in many countries, and health experts urge residents to get their jabs. Though the threat of new variants may affect vaccination efforts, protecting as many as possible can reduce the burden on healthcare systems.
Source:
Journal reference: