Twins may look alike on the outside, but not so much on the inside. That's one takeaway from a new preprint study posted to the medRxiv* server where Brazilian researchers observed different T-cell responses in two pairs of identical twins exposed to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). One twin who was reinfected with SARS-CoV-2 four months after had low recognition of CD4+ and CD8+ T-cell epitopes.
Given the danger of SARS-CoV-2 variants that can escape immunity, boosting T cell responses may be necessary to protect against reinfection.
Tracking the twins
The researchers investigated the immune response in two pairs of identical twins. One pair of twins had mild COVID-19 infection in early 2020, with the first twin becoming infected in February and another in April. Both were confirmed to have an immune response towards SARS-CoV-2 in mid-May 2020.
The first twin was a healthcare worker reinfected with a severe COVID-19 illness four months after recovering from the initial infection. The severity of the second infection caused the twin to undergo hospitalization in the ICU because of low oxygen levels. Her resulting IgG titer was two-fold higher than what she had in mid-May.
The second pair of twins had an asymptomatic infection and served as controls for the study.
The twins were tracked 6 to 10 months after presenting with COVID-19 symptoms. Blood samples were obtained in July 2020 for the first pair of twins and January 2021 for the second pair to measure innate and adaptive immunity.
Using the blood samples, they performed several binding and neutralizing antibody assays to measure the innate type I/III IFN response kinetics after TLR3 stimulation and the T cell response to SARS-CoV-2 synthetic peptides with the IFN gamma ELISPOT assay.
Immune responses in twins
Both twins had IgG titers that targeted the coronavirus spike protein. The first twin that was later reinfected presented with higher IgG titers and the second twin had anti-Spike and anti-NP IgG. The control twins who had asymptomatic infection showed similar neutralizing antibody levels to the reinfected twin.
All twin pairs had IgG antibodies against the receptor-binding domain of three of the four endemic coronaviruses: NL63, 229E, HKU1, and OC43.
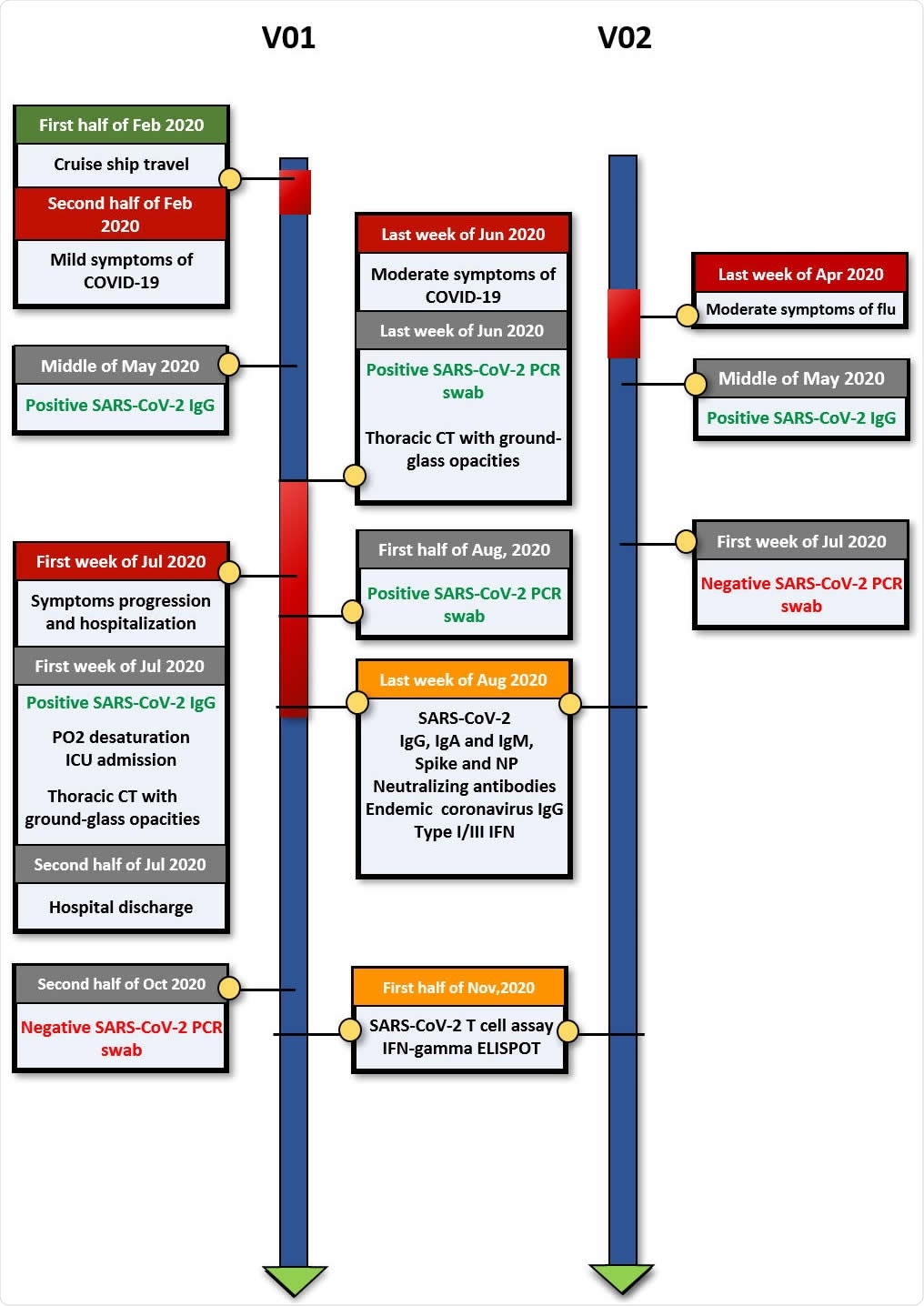
Timeline of clinical events, diagnostic results and blood draws for comprehensive immunological assessment. Pair 1
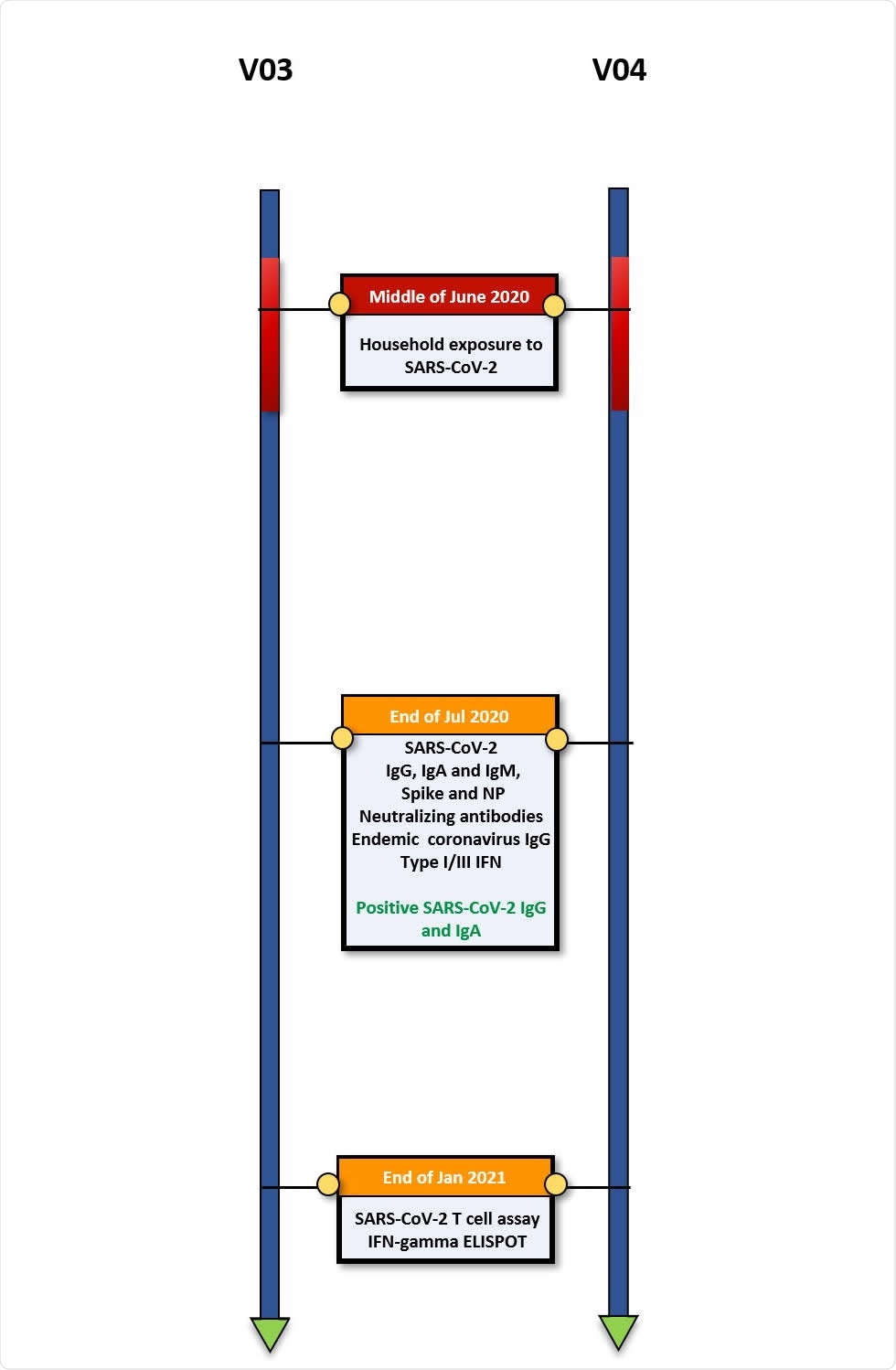
Timeline of clinical events, diagnostic results and blood draws for comprehensive immunological assessment. Pair 2.
Innate immunity towards SARS-CoV-2
The researchers next looked at the innate immunity to SARS-CoV-2 by assessing type I/III IFN — the first line of defense against RNA viruses. They observed early and high mRNA expression from one of four IFNs in all four cases.
The reinfected twin expressed high levels of IFNB1 while her sibling showed high levels of IFNA2 and IFNL3. One of the control twins showed high IFNA2 and INFL2, while the other showed increased expression of IFNB1.
Considering all four participants showed early and strong expression of type I/III IFNs suggests that reinfection is unlikely to be attributed to the IFN response.
Low T cell response observed in adaptive immunity
When evaluating T cell responses, they found a reduced number of T cell responses in the reinfected twin than her sibling. Only 3 out of 20 CD4+ T cell epitopes were identified in the reinfected twin, while 17 CD4+ T cell epitopes were recognized in the sibling. In addition, the reinfected twin had only 4 CD8+ T cell epitopes recognized compared to the 19 out of the 26 CD8+ T cell epitopes recognized by the sibling.
The control twin pair recognized more than 70% of both CD4+ and CD8+ T cell epitopes.
"These results indicate that the twin with COVID-19 recurrence showed a drastically reduced breadth (number of recognized epitopes) of both CD4+ and CD8+ SARS-CoV-2 T-cell epitopes as compared with her non-recurrent sibling and also the second MZ twin pair," wrote the researchers.
The team notes this is the first case of innate and T cell immune responses differing potentially because of SARS-CoV-2 reinfection. However, given the study's small sample size, more research is needed to assess whether this was indeed reinfection or a viral relapse. Future work can also help confirm whether the failure of a broad T cell response is a common mechanism for recurrent COVID-19 infection.
Important Notice
*medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.