Researchers in the UK have presented a multi-omics integrated blood atlas that delineates the host immune response in patients with coronavirus disease 2019 (COVID-19) of varying severity, providing a unique reference resource for the interpretation of datasets generated from interventional trials.
Through the COvid-19 Multi-omics Blood ATlas (COMBAT) consortium, David Ahern from the University of Oxford and colleagues characterized COVID-19 of varying severity and identified immune signatures and correlates of host response.
The team says that integrative approaches such as those applied here are essential to better differentiating COVID-19 patients according to disease severity, underlying pathophysiology and infectious etiology.
“Our systems-based integrative approach and blood atlas will inform future drug development, clinical trial design and personalized medicine approaches for COVID-19,” write the researchers.
A pre-print version of the research paper is available on the medRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
COVID-19 pathophysiology is highly heterogeneous between patients
The pathophysiology induced by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes COVID-19 – involves a complex interplay between lung pathology and maladaptive immune system responses.
Severe COVID-19 is characterized by hypoxia and can progress to acute respiratory distress syndrome, multiple organ failure and death.
Predisposing factors for severe disease include age, gender, ethnicity, obesity and comorbidities.
Currently, targeted precision treatment approaches are limited by an incomplete understanding of the clinical heterogeneity among patients and of the potentially druggable immune mediators of disease.
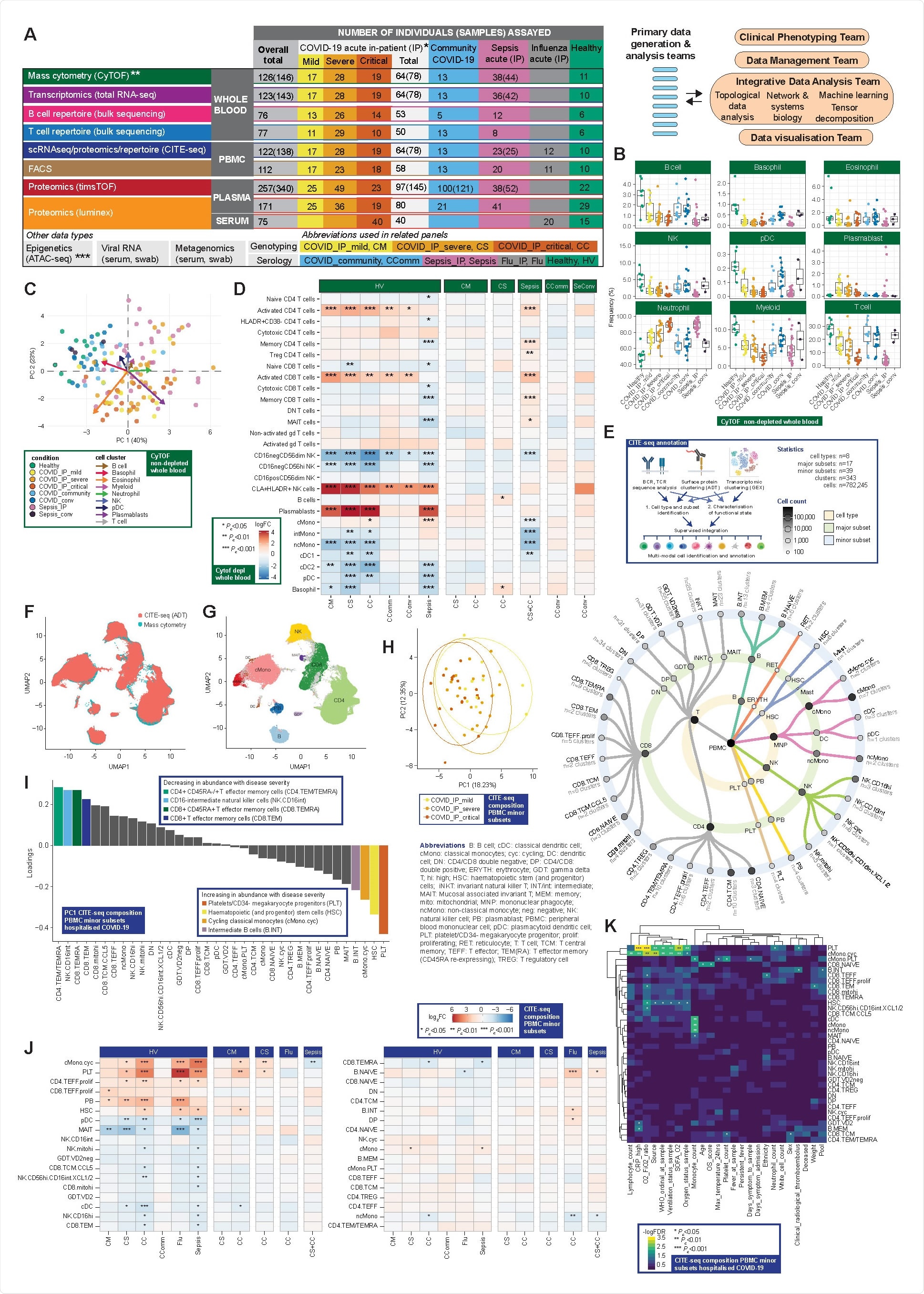
Complementary single cell compositional approaches reveal variance in specific cell populations by clinical group and severity (A) Study design, assay modalities and workflow. Table shows number of patients assayed, with number of samples in brackets where more than one sample assayed. *WHO severity categories show number of patients at time of sampling **single paired convalescent sample assayed for n=16 COVID-19 and n=3 sepsis patients; ***10 samples assayed (8 samples for paired acute-convalescent COVID-19 and 2 healthy). (B-G) Major cell populations in whole blood for clinical comparator groups assayed by single cell mass cytometry (CyTOF) showing (B,C) for non-depleted samples (3,893,390 cells) (B) cell frequencies (C) PCA with arrows indicating drivers of variation by cell population and (D) differential abundance analysis of CD66+ depleted whole blood (7,118,158 cells assayed) by patient group (E) multimodal identification and annotation of PBMC subpopulations based on curated intersection of CITE-seq data (F,G) UMAP showing joint visualization of CITE-seq and CyTOF datasets (using CITE-seq data as reference) (F) overlaid CITE-seq (ADT) and mass cytometry (G) cell annotations transferred between datasets and coloured by cell type where concordant (94.5% of cells) or discordant (grey). (H-K) CITE-seq compositional analysis of minor subsets (H,I) PCA for hospitalized COVID-19 cases (H) PC1 vs PC2 (I) analysis of loadings of minor subsets on PC1. (J) Differential abundance analysis between clinical groups (K) Covariate analysis for clinical, demographic and experimental variables for hospitalized COVID-19 cases (with BH adjusted ANOVA test for significance).
What did the researchers do?
Now, through the (COMBAT) consortium, Ahern and colleagues have used a comprehensive multi-omics blood atlas in patients with varying COVID-19 severity to identify cells, mediators and pathways that are hallmarks of increasing disease severity.
To characterize the peripheral blood response to COVID-19, the researchers analyzed a prospective cohort of adult patients with confirmed SARS-CoV-2 infection who presented to clinical services during February and March 2020 – at the start of the UK pandemic and prior to any implementation of approved treatments or vaccination.
The team recruited a prospective cohort of 116 patients hospitalized with COVID-19 at Oxford University Hospitals. Samples were collected during acute admission and from 28 days following hospital discharge of convalescent individuals.
Results from these samples were compared with those from recovering COVID-19 cases in the community who had not required hospitalization, age-matched healthy volunteers, influenza cases requiring intensive care, and all-cause sepsis patients.
What did they find?
The team’s comprehensive, multi-modal analysis of multiple well-defined patient cohorts and healthy volunteers identified blood hallmarks of COVID-19 severity and specificity involving particular immune cell populations, components of innate and adaptive immunity, and connectivity with the inflammatory response.
The team found evidence for increased levels of activated CD8+ T cells and natural killer cell populations in cases of COVID-19 and failed clonal expansion in CD8+ T effector and central memory cells as disease severity increased.
Proteomic analysis identified specific plasma cytokine and chemokine levels as biomarkers of severe disease, with evidence for the following as hallmarks: acute phase inflammation, complement activation, fibrin clots, proteases, serum amyloid, tissue necrosis, receptor-mediated endocytosis and cholesterol transport.
Plasma protein signatures could be used to stratify patients
The study revealed plasma protein signatures that can be used to stratify hospitalized patients with acute COVID-19 into disease sub-phenotypes, with cluster membership associated with differential 28-day mortality.
“Patient stratification is important given the observed clinical heterogeneity within severe COVID-19. Such variability has historically been a major confounder of clinical trials for targeted immune therapy in other severe infections,” writes the team.
The researchers also found that the ratio of integrin alpha 4 (CD49d) to leukosialin (CD43) is specifically elevated in COVID-19 patients, including into recovery and during convalescence.
Reduced CD43 expression has been shown to lead to neutrophil retention in the bloodstream and increased adherence to vessel walls, which may be linked to the enhanced thrombosis observed in COVID-19 patients.
The CD49d:CD43 ratio may be an informative index score for neutrophil activities specific to COVID-19, suggests Ahern and colleagues.
AP-1 p38 MAPK pathway upregulation was a specific feature of COVID-19
The analysis also identified upregulation of the AP-1 p38 MAPK pathway as a specific feature of COVID-19 disease across different immune subsets.
“Combined with evidence of proliferation and cytokine response in these populations, this supports systemic immune activation and proliferation as a hallmark specific to COVID-19,” write the researchers.
The team says this finding is in keeping with recent evidence that baricitinib improves the recovery of hospitalized patients. This drug has been shown to act upstream of AP-1 and to control macrophage inflammation and neutrophil recruitment in COVID-19.
What are the implications of the findings?
The researchers say the multi-omics integrated blood atlas presented here provides a unique reference resource for replication and meta-analysis for interpreting datasets generated from interventional trials and includes tools for direct visualization (https://mlv.combat.ox.ac.uk/).
“Integrative approaches such as we have applied here are essential to better differentiate COVID-19 patients according to disease severity, underlying pathophysiology and infectious etiology,” writes Ahern and colleagues.
“This will be important as we seek novel therapeutic targets and the opportunity for a precision medicine approach to treatment that is appropriately timed and targeted to those patients most likely to benefit from a particular intervention,” concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources