Positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) tests are frequently obtained from individuals that have already recovered from the virus in the past. They have therefore undergone seroconversion and bear the expected antibodies.
It is unclear whether the majority of these positive cases are indicative of reinfection, prolonged viral clearance, or are common false positives as a consequence of the type of test employed.
Whatever the reason, this makes studying the occurrence and effectiveness of natural immunity difficult in a broader population.
In a research paper recently uploaded to the preprint server medRxiv* by Isaac S. Kohane et al. (May 18th, 2021), 4.2 million test results from the USA were analyzed, identifying a common pattern among those with apparent reoccurring SARS-CoV-2 infection.
How was the study performed?
Data were collected from outpatient laboratories and insurance providers across the United States.
Only participants that had received two positive RT-PCR tests for SARS-CoV-2 at least 42 days apart, a typical viral shedding period, with an intervening serological IgG test were included in the study.
The serological test was intended to demonstrate that patients had or were undergoing seroconversion, and were therefore in recovery. To better account for false positives, the sensitivity of the RT-PCR and serological tests was raised to 98% and 91%, respectively, and the specificity of both to 99.5%.
Of the over 200,000 patients examined with a positive RT-PCR test, only 79 were found by the group, with a second positive test occurring over six weeks later and a positive serological test in-between. The group notes that several of these individuals had multiple positive tests in this period.
However, the data privacy restrictions of the study precluded them from contacting any participants to confirm reinfection.
Analyzing the data
The average number of days between a positive serological test and the second positive RT-PCR test among these 79 individuals was 21, though some were recorded as shortly after as the next day.
It was also observed that these patients had more comorbidities than average, which indicates that a compromised immune system might make reinfection or slow shedding more likely.
Comorbidities most likely to influence patients included high cholesterol, hypertension, obesity, diabetes, and heart failure, with 75% of patients being older than 44.
In this study, the average age of the participants was 55, and the likelihood of shedding or reinfection decreased with age.
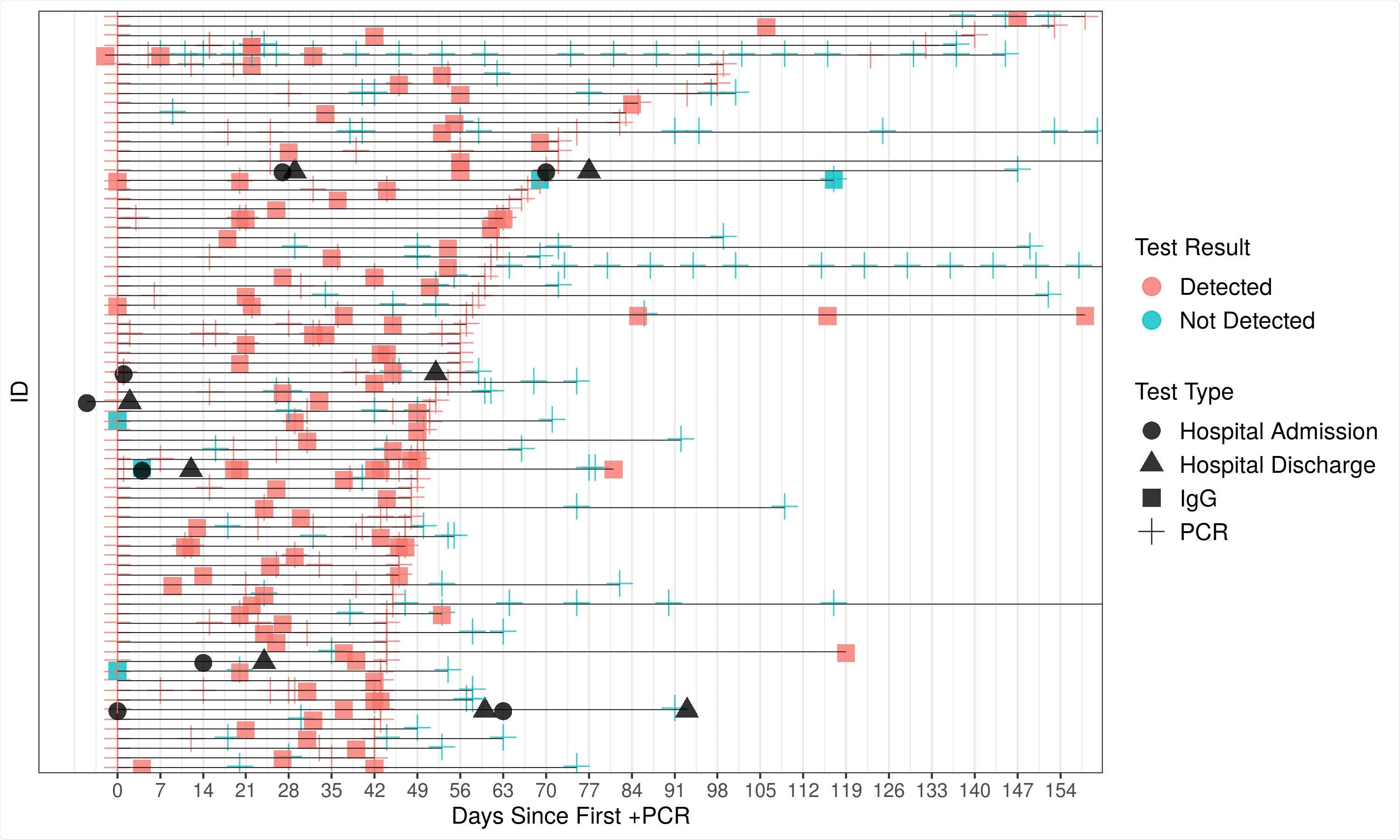
Timeline of tests for individuals with potential reinfection or prolonged viral shedding. That is, patients with the testing pattern, positive PCR, positive IgG, positive PCR with the two positive PCR tests separated by at least 42 days.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
However, it is likely that selection bias occurred, with the average age of PCR testing being notably lower than 55, and older patients than this bearing significantly greater mortality risk, therefore being unable to receive a second test.
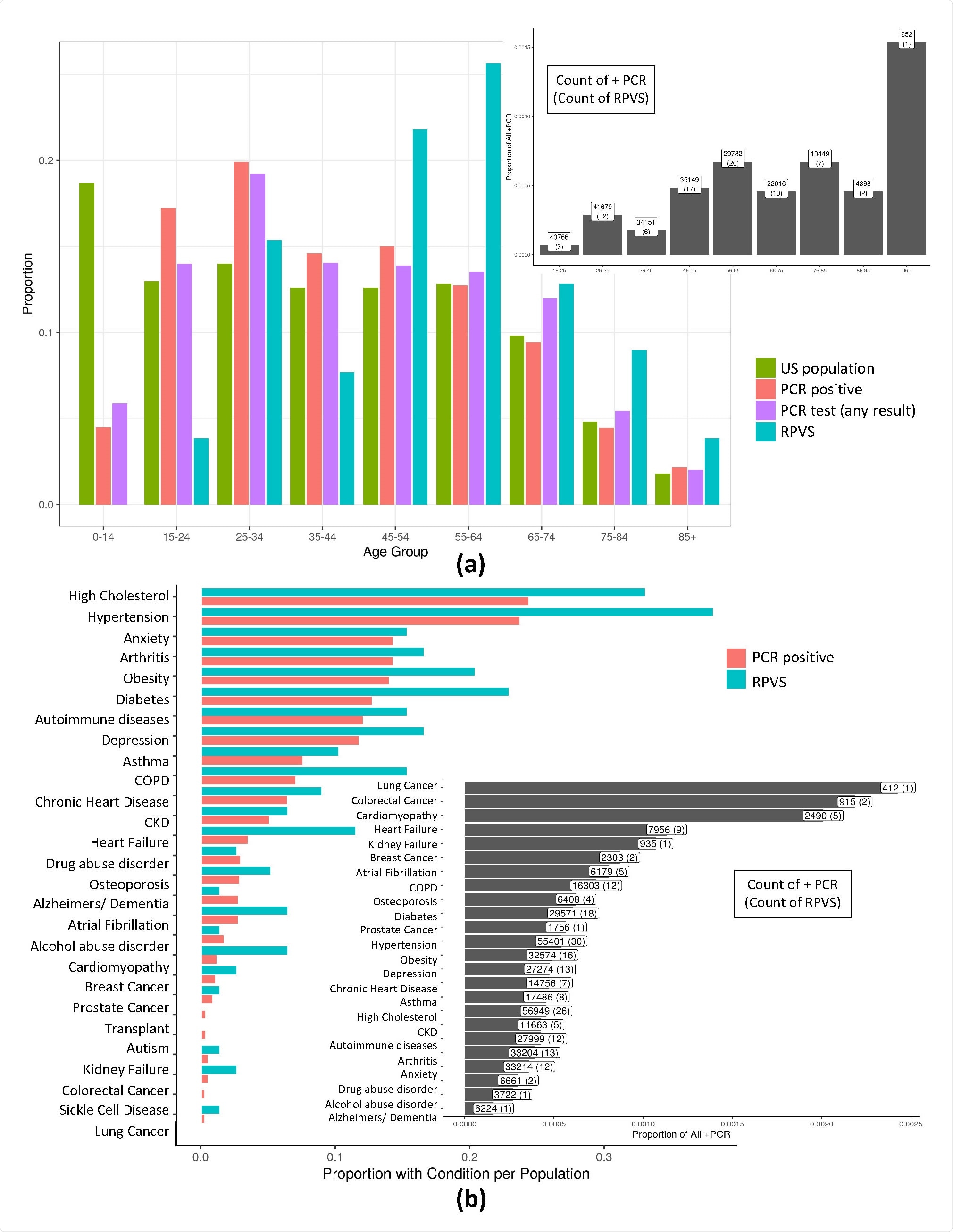
a) A normalized histogram of the US population, all those with a PCR test result in our database, those with a positive PCR test result, and suspected reinfection or prolonged viral shedding cases across patient age. For RPVS patients the median age is 56, and average is 54.65. In particular, 75% of cases are from age group above 44 suggesting a possible increased susceptibility to an RPVS state with age. Of note, this advanced age is not due to an ascertainment bias due to testing frequency with age since the highest group for per capita testing is aged 25-34. Further, RT-PCR positive cases (median = 42, average = 43.46) is shifted towards the younger ages relative to the putative RPVS cases. Further, the inset shows RPVS cases normalized by PCR positive cases in each age group. b) Histogram of comorbid conditions of those with COVID-19 (PCR positive) and RPVS patients. Again, the inset shows RPVS cases normalized by PCR positive cases for each comorbid condition
Overall, Kohane et al. state that these tests are unlikely to be false positives, and the observed pattern of infection-serological conversion-apparent reinfection is valid, though more probably associated with delayed or long-term viral shedding in immune-compromised individuals than reinfection.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.