Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread worldwide, and its airborne transmission makes it easy to infect a person even if there is a lack of symptoms. The Centers for Disease Control and Prevention (CDC) COVID-19 Response Team, led by Martin I. Meltzer confirmed that contact tracing helps reduce COVID-19 cases by shortening the time between testing and self-isolation. The current research shows case investigation and contact tracing prevented between 4 and 97 additional cases for every 100 COVID-positive cases.
These findings may influence how health policies are framed and help improve contact tracing efforts in places where it may take a long time before contacting people who have been exposed to an infected person. The researchers write:
“Our modeled estimates indicate that reducing the time from notification of a positive test result and the subsequent isolation and quarantine of cases and contacts (even by just 1 day) provides the biggest gain in improving the impact of CICT. We found this to be true even when compared to the potential impact of a 20% increase in percentage of cases interviewed or contacts notified and monitored for compliance with quarantine recommendations.”
The study “Estimates of cases and hospitalizations averted by COVID-19 case investigation and contact tracing in 14 health jurisdictions in the United States” is available as a preprint on the medRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Model estimates of case investigation and contact tracing
The team used a public tool called COVIDTracer Advanced to estimate the rate of quarantine of close contacts to someone exposed to COVID. They also collected data — interviewed cases, the number of contacts notified or monitored, and how soon people tested for COVID were notified of their status — from 14 jurisdictions to model how contact tracing affected the rate of COVID-19 cases and hospitalizations in 60 days.
Time taken to self-isolate and to notify close contacts to quarantine was a considerable factor influencing the number of cases and hospitalizations in an area. The researchers suggest reducing the time it takes to contact a person of a possible case exposure by a day could prevent about 15% of COVID-19 cases and COVID-related hospitalizations.
As many as three to six cases and hospitalizations could be avoided if 20% more COVID-19 positive interviews and information on their contacts were obtained.
The researchers estimated that locations that already had a longer turnaround time being notified of possible COVID exposure and quarantining would benefit the most from these changes.
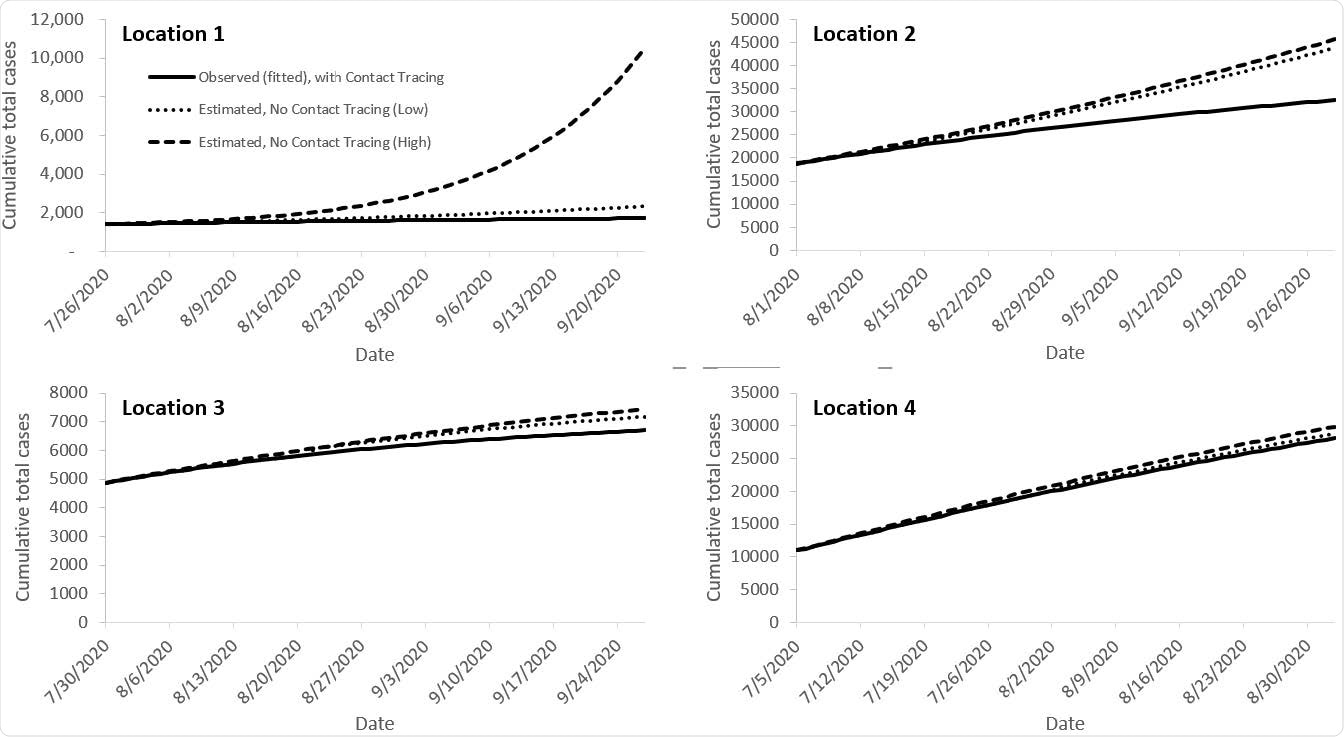
Epidemic curves fitted to observed case counts with case investigation and contact tracing programs, and estimated cases illustrating what might have occurred had the programs not been implemented
Study limitation
The study assumed people who were contacted complied with quarantine guidelines — though there’s a possibility people ignored or did not fully isolate as required by their health departments. As a result, the results could overestimate the usefulness of contact tracing.
Despite the study limitation, the researchers suggest the results reflect the benefits of contact tracing when there is high public compliance for quarantining.
The team also aggregated data but did not differentiate whether some contact tracing efforts came from smartphone-enabled contact tracing apps, which could influence how accessible some contact tracing methods were and other results.
The contact tracing data from COVIDTracer Advanced grouped all hospitalizations for all 14 locations used for the modeling study. Areas with an older population could have changed the rate of hospitalizations in specific locations.
“As such, we may overestimate or underestimate the hospitalizations prevented. We believe, however, that it is unlikely that incorporating location-specific precision on hospitalizations would yield any different policy choices,” argued the researchers.
Potential changes in COVID-19 contact tracing policies
Based on the evidence of reducing COVID-19 cases, the researchers recommend optimizing contact tracing to reduce the spread of SARS-CoV-2. The benefit will be most observable in areas where there’s a long delay between a COVID-19 exposure and quarantining of close contacts.
Time should also be allocated away from numbers that cannot be reached to prioritizing cases and contacts who were recently tested or people who have early symptoms indicating infection. The team also advises limiting time spent on the call to reach more people, either by asking fewer questions or sticking to a shorter script.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Jeon S, et al. Estimates of cases and hospitalizations averted by COVID-19 case investigation and contact tracing in 14 health jurisdictions in the United States. medRxiv, 2021. doi: https://doi.org/10.1101/2021.05.27.21257931, https://www.medrxiv.org/content/10.1101/2021.05.27.21257931v1
- Peer reviewed and published scientific report.
Jeon, Seonghye, Gabriel Rainisch, R. Ryan Lash, Patrick K. Moonan, John E. Oeltmann, Bradford Greening, Bishwa B. Adhikari, and Martin I. Meltzer. 2021. “Estimates of Cases and Hospitalizations Averted by COVID-19 Case Investigation and Contact Tracing in 14 Health Jurisdictions in the United States.” Journal of Public Health Management and Practice Publish Ahead of Print (September). https://doi.org/10.1097/phh.0000000000001420. https://journals.lww.com/jphmp/Fulltext/2022/01000/Estimates_of_Cases_and_Hospitalizations_Averted_by.5.aspx.