Researchers have evaluated 3D printed sample collection swabs made in-house and found them to be a reliable alternative to commercial swabs.
The detection of coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is done by collecting samples from the nose and throat. The samples are usually collected using a swab, which has fibers that help better the collection and transport of the sample. As the pandemic continues throughout the world, there is a shortage of testing reagents and sampling swabs, leading to delayed results, affecting the spread of the virus.
To overcome the supply challenge, 3D printing technology was used to rapidly build prototypes. Several teams made available open-source designs for making 3D printed swabs, and workflows were established for local printing.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Researchers from the Université de Montréal and the Université du Québec in Canada evaluated the fabrication process and clinically tested 3D printed swabs manufactured within a hospital, comparing them with commercially available swabs. They reported their results in a paper published on the medRxiv* preprint server.
Evaluating swabs
The swabs were 3D printed locally at the hospital system using the designs provided by the University of South Florida and the Northwell Health system, sterilized and immediately packed individually. The team tested the swabs at their institution’s COVID-19 screening clinic.
From the two designs available, the team selected one that had a smaller head size and greater flexibility for clinical tests. To this design, they added a breaking point some distance from the tip to enable storage and transport of the swab head with the sample.
They ensured that the swab heads were sterile by inoculating the swabs with a bacteria, subjecting them to the sterilization procedure, and testing them for bacterial growth. If the sterilization procedure was effective, no bacteria would grow on the inoculated swabs.
The team tested the swabs on 63 patients, about half of who tested negative for COVID-19. They used 3D printed swabs from three different lots for collecting samples. They found no significant statistical difference in the cycle threshold counts between the PCR results obtained using the 3D printed swabs or the commercial swabs. The overall agreement between the data obtained from the two different swabs was about 97%. The data for the two samples did not agree with each other.
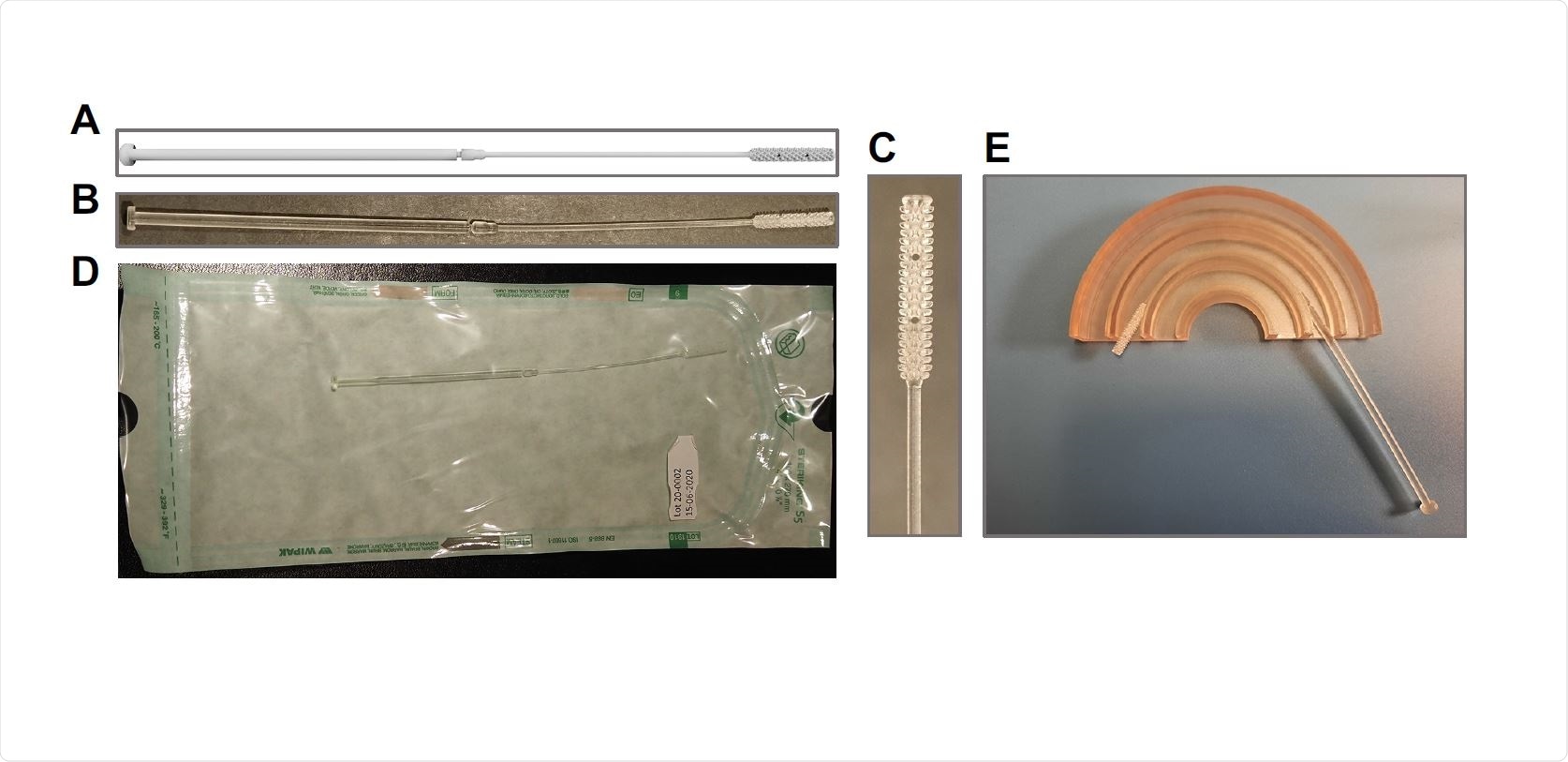
In-house 3D printed swab model. Design of the Northwell 3D swab model with the addition of a breakout point (A) used to 3D-print swab in our hospital (B and C). Swabs were individually packed in autoclavable and vacuum-sealed poches (D) for sterilization. (E) Flexibility was mechanically tested using semicircular canals (radius of 15, 25 and 35 mm).
Potential replacement for commercial swabs
The results indicate that if there is a shortage of commercial swabs, 3D printed swabs may be used to collect samples. This finding corresponds to results from previous studies comparing 3D printed swabs with commercial swabs.
The authors were able to take advantage of their health-related 3D printing center in their institution along with sterilization services, which allowed them to quickly perform steam sterilization. Because of the available setup and presence of staff, the cost per 3D printed swab was about 56 US cents. Further optimization can lead to increased production volume and lower production costs.
Our clinical trial has demonstrated that our local 3D printed swab production line offers a reliable local alternative to commercial swabs and therefore confirms that it is a viable local response to provide replacements in the event of pandemic supply chain disruption,” write the authors.
With SARS-CoV-2 continuing to spread in many parts of the world, there will be a need for increased testing capacity. Such local methods for making sample collection swabs may help with increased testing.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Lapierre, S. G. et al. (2021) Clinical Evaluation of In House Produced 3D Printed Nasopharyngeal Swabs for COVID-19 Testing. medRxiv. https://doi.org/10.1101/2021.05.26.21257548, https://www.medrxiv.org/content/10.1101/2021.05.26.21257548v1.
- Peer reviewed and published scientific report.
Grandjean Lapierre, Simon, Stéphane Bedwani, François DeBlois, Audray Fortin, Natalia Zamorano Cuervo, Karim Zerouali, Elise Caron, et al. 2021. “Clinical Evaluation of In-House-Produced 3D-Printed Nasopharyngeal Swabs for COVID-19 Testing.” Viruses 13 (9): 1752. https://doi.org/10.3390/v13091752. https://www.mdpi.com/1999-4915/13/9/1752.