A team of scientists from the Columbia University, New York, has recently identified a potential biomarker to predict acute kidney injury in coronavirus disease 2019 (COVID-19) patients. By analyzing urine samples of 444 COVID-19 patients, they have revealed that the urinary level of neutrophil gelatinase-associated lipocalin (NGAL) can be used to determine the severity and duration of acute kidney and tubular injuries, as well as to predict the risk of mortality in acute COVID-19 patients. The study is currently available on the medRxiv* preprint server.
Elevated serum level of creatinine is a commonly used marker to predict acute kidney function loss in patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). However, it is not a reliable maker to diagnose subtotal kidney damage or kidney injuries in the early stages. Moreover, the anatomical and physiological causes of kidney function loss cannot be predicted by serum creatinine levels.
According to the literature, urinary NGAL and kidney injury marker-1 (KIM-1) are two sensitive markers for detecting kidney and tubular injuries. Since these two molecules are derived from different segments of the kidney, they can accurately differentiate between volume depletion and acute tubular injury in real-time.
Given these observations, the scientists from the Columbia University have investigated whether urinary levels of NGAL and KIM-1 can detect acute kidney and tubular injuries in COVID-19 patients, as well as predict the clinical consequences of the disease.
Study design
The scientists collected urine and blood samples from 444 patients who tested positive for SARS-CoV-2 via reverse transcription-polymerase chain reaction (RT-PCR). The samples were collected immediately after hospital admission and within 1 day of a positive viral test in 70% of patients.
In the urine samples, NGAL, KIM-1, and proteinuria were measured, and the levels were correlated with the clinical data. The baseline serum creatinine was determined for each patient by assessing previously available data. A more than 50% increase in serum creatinine from the baseline was interpreted as a loss of kidney excretory function (acute kidney injury).
The stages of acute kidney injury were determined using serum creatinine kinetics. From the baseline, 1.5 to 2-fold, 2 to 3-fold, and more than 3-fold increase in serum creatinine levels were considered as stage 1, stage 2, and stage 3 acute kidney injury, respectively.
Important observations
At admission, the COVID-19 patients with acute kidney injury or sustained acute kidney injury exhibited significantly higher urinary levels of NGAL compared to those without kidney injury. A positive correlation was also observed between the NGAL levels and increasing stages of acute kidney injury. Specifically, the analysis revealed that NGAL had 80% specificity and 75% sensitivity to diagnose higher stages of acute kidney injury.
Furthermore, urinary NGAL as a predictive marker for acute kidney injury was independent of the patient’s age, sex, ethnicity, baseline creatinine level, proteinuria, and pre-existing health conditions.
Regarding clinical consequences of COVID-19, urinary NGAL quantitatively predicted the risk of in-hospital mortality, duration of hospital stay, shock, and acute dialysis. Per standard deviation of NGAL, the risk of death increased by 73% in COVID-19 patients. Specifically, in patients with the highest urinary NGAL, about 25% mortality was observed within 20 days of hospital admission. This risk prediction was independent of the patient’s demographic features, comorbidities, proteinuria, and baseline creatinine level.
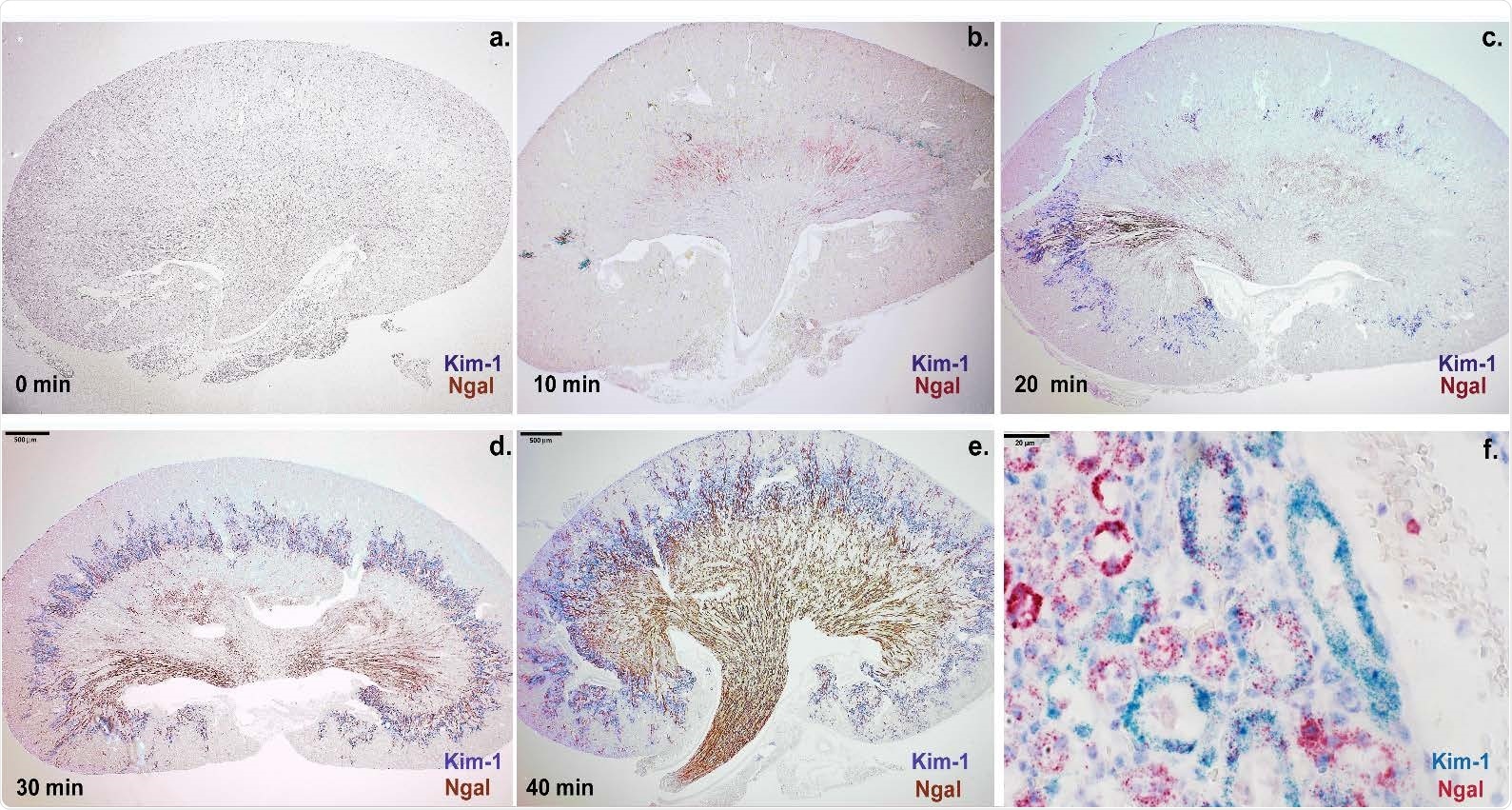
The expression level of Ngal (red-brown) and Kim-1 (blue-purple) depended on the dose of arterial ischemia in mouse: (a-e) Ngal expression was found at the cortico-medullary junction after 10min of ischemia, but throughout the medulla and papilla after 30-40min of ischemia. Kim-1 expression was found in the cortex and throughout the cortico-medullary junction. (e-f) Prolonged ischemia (40min) broadened the expression domain of Ngal to include the proximal tubule marked by Kim-1. In contrast to Ngal, Kim-1 expression remained localized to the cortex and cortico-medullary junction. Bars a-e: 500μm; Bars f: 20μm.
Unlike urinary NGAL, the levels of urinary KIM-1 failed to significantly detect the duration and severity of acute kidney injury and predict the clinical outcomes in COVID-19 patients.
In a separate set of examinations on 13 COVID-19 patients and 4 non-COVID patients with acute tubular injury, the transcriptomic analysis of NGAL and KIM-1 was conducted in different segments of the nephron. The findings revealed that in both COVID and non-COVID patients, KIM-1 and NGAL were predominantly expressed in the proximal tubule and in the limbs of Henle and collecting ducts, respectively.
In COVID-19 patients with maximum acute kidney injury, KIM-1 and NGAL were expressed in 27% and 66% of tubules, respectively, indicating a widespread distribution of NGAL compared to KIM-1. Moreover, an extensive co-expression of NGAL with KIM-1 was observed in the proximal tubule. Importantly, a significant correlation was observed between the NGAL – KIM-1 co-expression and degree of acute kidney injury.
To further investigate the NGAL distribution, the expression of NGAL at the RNA level was determined in mice with renal ischemia reperfusion injury. The NGAL RNA was found to express in the cortico-medullary junction, medulla, and papilla. Moreover, an overlap between NGAL and KIM-1 was observed in the proximal tubule.
Study significance
The study identifies urinary NGAL as a potential marker for determining the duration and severity of acute kidney injury, as well as predicting clinical outcomes in COVID-19 patients.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources