COVID-19 pandemic containment in the U.S. began in early 2020 with rigorous nonpharmaceutical interventions such as stay-at-home orders and remote-work directives. During this period, surveys and wearable data reported an increase in sleep duration and delayed sleep timing, as well as a spike in adverse mental health symptoms.
Now, a group of researchers from the USA and Australia recently collaborated on a study analyzing objective sleep-wake data and the effect of COVID-19 on the mental health of adults in the USA.
A pre-print version of the research paper is available on the medRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Impaired sleep and mental health
The importance of sleep for mental health has long been established, with associations between impaired sleep, including sleep disturbances and insufficient sleep, and adverse mental and behavioral health symptoms. For some people, these symptoms include anxiety, depression, and substance abuse.
It was inescapable that COVID-19 would have adverse effects on mental health, owing to the isolated lifestyle and low social interaction associated with the pandemic.
In order to mitigate the spread of the virus and reduce the possibility of infection, lockdowns have been implemented globally as a stringent mitigation measure.
As a result, interdisciplinary research priorities focused on identifying optimal sleep-wake structures to support mental health in the wake of isolating effects with subsequent depressive and anxious states.
Survey data that analyzed the initial phase of COVID-19 had found links between poor quality, insufficient sleep, and having adverse mental and behavioral health symptoms.
The research published in the current pre-print has examined the objective sleep and mental health among 20,717 individuals residing in the United States through the use of a validated sleep wearable, both prior to COVID-19 as well as during the pandemic.
The researchers used a comprehensive list of variables for their sleep study which included, duration, sleep onset, sleep offset, consistency of sleep timing and wake after sleep onset.
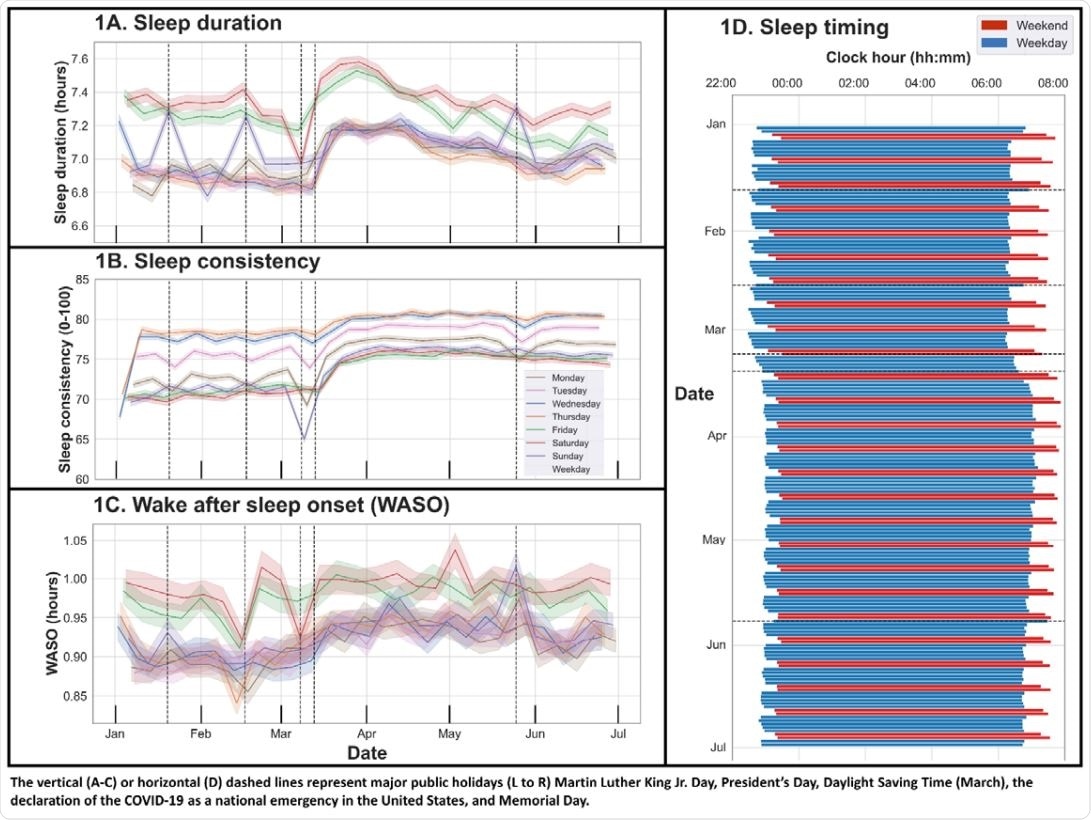
Sleep duration, consistency, wake after sleep onset, and timing, January 1, 2020—June 30, 2020.
The significance of sleep
The study's findings confirmed previous research studies on the quality of sleep and the state of mental health, with results demonstrating that there had been an increase in sleep duration within the pandemic and a delay in sleep timing.
The research, however, revealed new findings concerning the consistency of sleep timing. In the study, it was found that those with persistent sleep problems and low sleep consistency were more likely to experience adverse mental health.
Mental health resilience
Sleep duration of 6-7 hours is considered normal, however, when this number is below 6, anxiety and depression symptoms are more likely to occur. This is also the case for decreased consistency of sleep timing. Based on these results, it can be seen that sleep plays a significant role in mental health as well as what behavioral interventions can do to increase resilience during the pandemic for the people most affected.
The study suggested the COVID-19 directives such as remote working from home and a lack of social mixing had contributed to the isolation faced by individuals to a significant degree.
The differences in sleeping patterns found by the researchers during the pandemic have identified potential targets for risk factors for mental health problems.
Research has found that individuals who achieved the recommended sleep duration and consistency prior to the pandemic had greater mental health resilience since they were less affected by sleep decline during the pandemic and therefore were less likely to manifest mental and behavioral symptoms.
Limitations
The limitations of the research, which is included in the pre-print paper, include the participants being predominantly male, highly educated, employed, and had reported a higher than average household income. This can be seen as a bias for the study, which may prevent the research from being representative of the population.
The socio-economic implications of this can be significant with women, racial diversity and different wealth brackets being excluded. The biological and social differences in women may have caused varying implications on sleep; this can also be said for how different races and less economically stable individuals may have handled the pandemic, with lost jobs and lack of security during a challenging period of time. This may have further affected sleep patterns during the pandemic and enhanced mental and behavioral symptoms in these individuals.
The research undertaken has provided a comprehensive insight into the challenges faced by a group of individuals in the USA. This can be used for mental health interventions to direct these for the most vulnerable groups during the pandemic. This can assist further with aiding the ease out of the pandemic and how groups of individuals can be provided with mental health support during COVID-19.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Czeisler, M., Capodilupo, E., Weaver, M., Czeisler, C., Howard, M. and Rajaratnam, S., 2021. Prior sleep-wake behavior predicts mental health resilience among adults in the United States during the COVID-19 pandemic. https://www.medrxiv.org/content/10.1101/2021.06.15.21258983v1
- Peer reviewed and published scientific report.
Czeisler, Mark É, Emily R Capodilupo, Matthew D Weaver, Charles A Czeisler, Mark E Howard, and Shantha MW Rajaratnam. 2022. “Prior Sleep-Wake Behaviors Are Associated with Mental Health Outcomes during the COVID-19 Pandemic among Adult Users of a Wearable Device in the United States.” Sleep Health, April. https://doi.org/10.1016/j.sleh.2022.03.001. https://www.sciencedirect.com/science/article/pii/S2352721822000183?via%3Dihub.