Systematic reviews of COVID-19 disease have reported a wide range of symptoms and the prevalence of persistent symptoms following severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
A review of long COVID studies conducted in March 2021 summarized the available literature on the persistent symptoms after acute COVID-19. The review also reported that most studies included hospitalized patients who had a higher prevalence of persistent symptoms compared to two community-based studies.
Long COVID describes the long-term sequelae after SARS-CoV-2 infection and remains poorly understood to date, with uncertainty about the predisposing factors and the extent of the public health burden caused by long COVID.
“There was limited evidence from community studies beyond 12 weeks.”
Large community-based study involving over half a million adults in England analyzes persistent symptoms following SARS-CoV-2 infection
UK-based researchers recently conducted a community-based study among more than half a million people; it was designed to be representative of the adult population in England. A random sample of adults 18 years and above who were registered with a GP were invited to participate in the study regardless of previous access to COVID-19 services to provide an estimate of population prevalence representative of the whole population.
This study is published on the medRxiv* preprint server while awaiting peer review.
Using rounds 3–5 of the REACT-2 study, a total of 508,707 people in the community in England were surveyed about prior history of COVID-19 and the presence and duration of 29 related symptoms. They used uni- and multivariable models to identify predictors of symptom persistence at 12 weeks or beyond.
Results show two distinct clusters with varying symptom profiles and identify risk factors for persistent symptoms at 12 weeks or beyond
The study's findings show significant declines in symptom prevalence during the first 12 weeks following SARS-CoV-2 infection, as reported by about 1/5th of the respondents. However, among these respondents, more than a third remained symptomatic at 12 weeks and beyond, with little evidence for decline thereafter. The weighted prevalence of self-reported COVID-19 among the 508,707 participants was 19.2%. While 37.7% of 76,155 symptomatic individuals post COVID-19 experienced at least one symptom, 14.8% experienced three or more symptoms that lasted 12 weeks or more.
Risk factors identified for persistent symptoms at 12 weeks or beyond, which is suggestive of long COVID, were female sex, obesity, and hospitalization due to COVID-19, with strong evidence for the risk increasing with age. There was also additional evidence for an increased risk in lower-income, smoking / vaping, and healthcare worker populations. People of Asian ethnicity were found to have a lower risk.
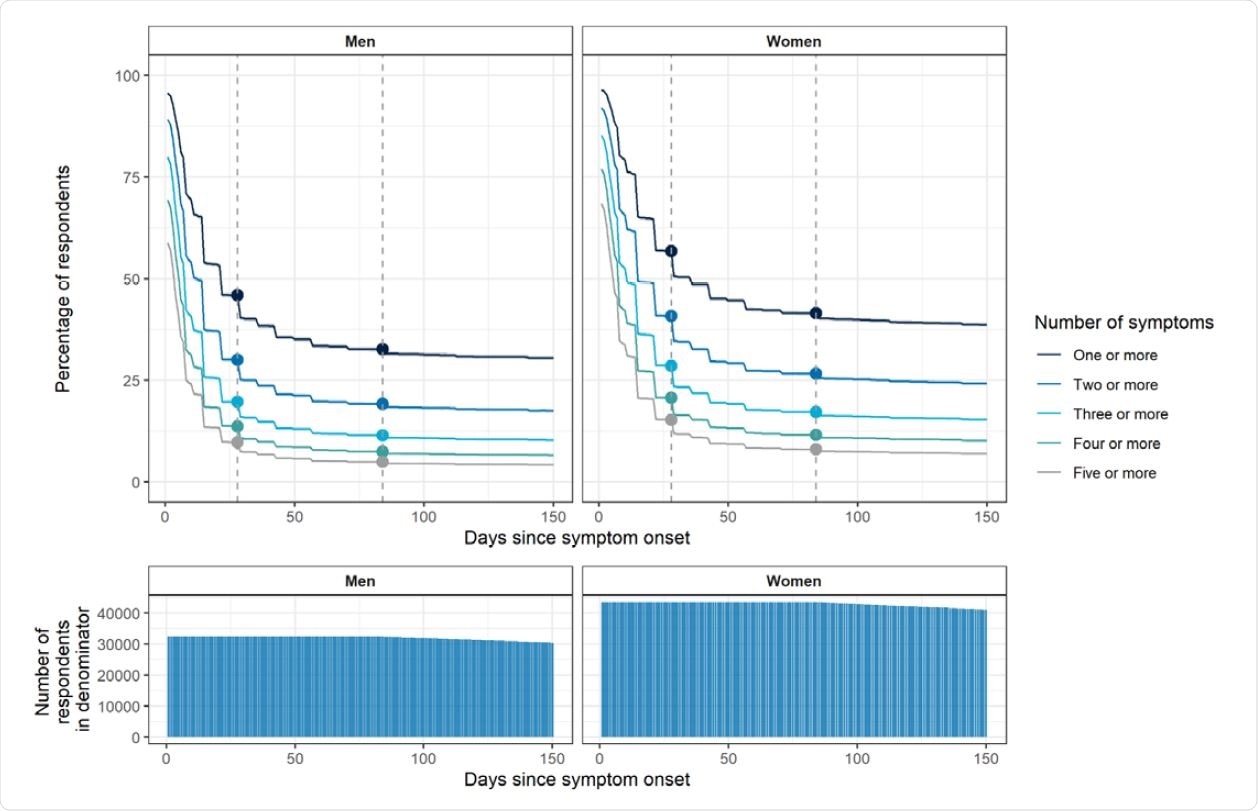
Plots showing persistence of symptoms as a proportion of those who reported symptoms at any time· Plots account for ‘censoring’ – i.e. the denominator in the proportion at day X is the number of respondents who reported a symptomatic infection X or more days prior to responding to the REACT-2 survey (the denominator is shown in the bottom panel plots). Women have higher rates of persistent symptoms; a slower decline in symptom prevalence is observed after 12 weeks in both sexes. The vertical dashed lines show 4 and 12 weeks.
Two distinct groups of individuals with varying symptom profiles at 12 weeks were identified by clustering, highlighting the heterogeneity of clinical presentation among the study population. The smaller cluster was found to have a higher prevalence of respiratory and related symptoms. In comparison, the larger cluster had tiredness as the dominant symptom and a lower prevalence of organ-specific symptoms.
“A substantial proportion of people with symptomatic COVID-19 go on to have persistent symptoms for 12 weeks or more, which is age-dependent.”
Distinct clusters of persistent symptoms highlight the need for recognition and management of these symptoms outside specialized services
From the findings, the high prevalence of persistent symptoms beyond 12 weeks post-acute COVID-19 infection, with little evidence for decline thereafter, highlights the need for increased specialized services support for these patients and financial support for those from low-income settings.
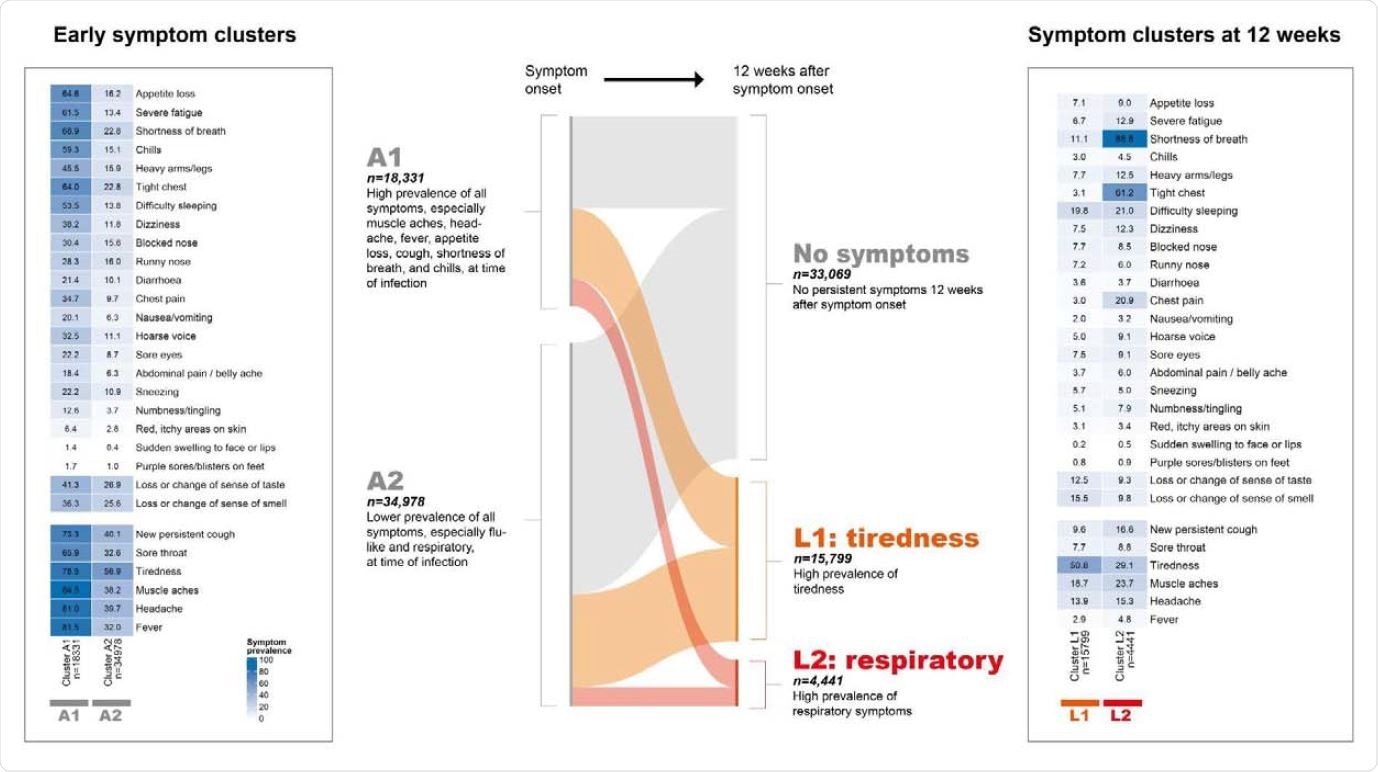
Results of clustering on symptom profile at time of symptom onset and then reclustering at 12 weeks, using CLARA (partitioning around medoids) algorithm. Central Sankey plot shows transitions between early and 12-week clusters. Two stable clusters of symptomatic infections were identified at t0: cluster A1 was characterized primarily by higher prevalence of flu-like symptoms (muscle aches, headache, fever, appetite loss, chills) and respiratory symptoms (shortness of breath, tight chest, new persistent cough). Two stable clusters were identified at 12 weeks. Cluster L1 (“tiredness cluster”) had high prevalence of tiredness. Cluster L2 (“respiratory cluster”) was a smaller subset of 4,441 participants who had high prevalence of shortness of breath and tight chest as well as chest pain.
According to the authors, the distinct clusters of persistent symptoms, the most common one being fatigue, are key evidence for the recognition and clinical management of the fatigue outside of specialized services. Health care providers need to be aware of the various manifestations of long COVID as they may require tailored therapeutic approaches.
“Managing the long-term sequelae of SARS-CoV-2 infection in the population will remain a major challenge for health services in the next stage of the pandemic.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Persistent symptoms following SARS-CoV-2 infection in a random community sample of 508,707 people Matthew Whitaker, Joshua Elliott, Marc Chadeau-Hyam, Steven Riley, Ara Darzi, Graham Cooke, Helen Ward, Paul Elliott, medRxiv, 2021.06.28.21259452; doi: https://doi.org/10.1101/2021.06.28.21259452, https://www.medrxiv.org/content/10.1101/2021.06.28.21259452v1
- Peer reviewed and published scientific report.
Whitaker, Matthew, Joshua Elliott, Marc Chadeau-Hyam, Steven Riley, Ara Darzi, Graham Cooke, Helen Ward, and Paul Elliott. 2022. “Persistent COVID-19 Symptoms in a Community Study of 606,434 People in England.” Nature Communications 13 (1): 1957. https://doi.org/10.1038/s41467-022-29521-z. https://www.nature.com/articles/s41467-022-29521-z.