Researchers in Sweden have challenged the interpretation that variable non-pharmaceutical interventions (NPIs) and “herd immunity” protection are responsible for the rise and fall of coronavirus disease 2019 (COVID-19) epidemic waves in hard-hit locations where authorities have not enforced strict NPIs.
However, the team’s study also indicates that these thresholds are unstable and cannot be considered indicative of protection against emerging variants of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes COVID-19.
“Vaccination roll-out must continue with high participation,” says Marcus Carlsson from Lund University in Scania and Cecilia Soderberg-Naucler from the Karolinska Institute in Stockholm.
A pre-print version of the research paper is available on the medRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Sweden provides a good example for testing mathematical models
In March 2020, mathematical models predicting the epidemiology of the COVID-19 outbreak had a significant impact on public policy.
For example, the imperial college report no. 9 predicted that 500,000 deaths would occur in the UK under the worst-case scenario, given that the government did not take any actions to mitigate the pandemic. This led to a shift in strategy towards curbing SARS-CoV-2 transmission and eventually a nationwide lock-down on March 23rd.
By contrast, the Swedish government kept society relatively open and only maintained limited but rather fixed NPIs throughout the pandemic.
This makes Sweden an excellent example for testing the validity of such mathematical models, say the researchers.
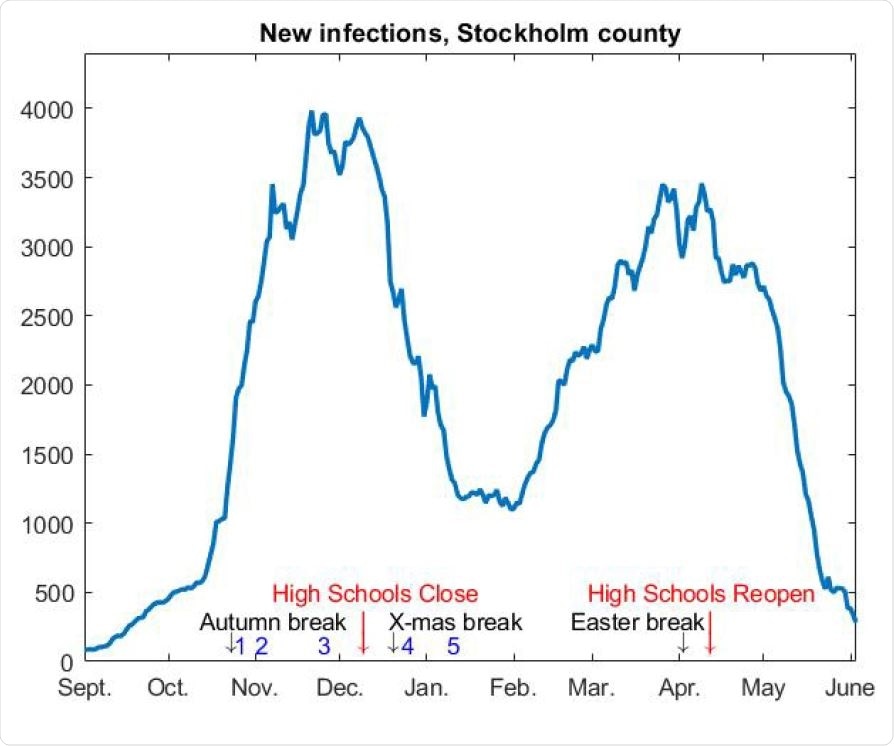
7-day rolling average of new cases in Stockholm county, adjusted to match the current seroprevalence.
What did the researchers do?
Carlsson and Soderberg-Naucler developed a mathematical model that took pre-immunity, antibody waning, and variants of concern into consideration.
This provided a theoretical framework for predicting SARS-CoV-2 cases in Stockholm without factoring in variable restrictions or vaccination roll-out.
Analysis of the time series of individuals who tested positive for SARS-CoV-2 in the Stockholm metropolitan area since September 1st, 2020, showed that two distinct epidemic waves followed the first wave that occurred in the Spring of 2020.
Before the second wave arose, the SARS-CoV-2 seroprevalence was around 10%. This rose to 22.6% after the second wave, but before the third wave was initiated. By extrapolation, this gives a seroprevalence of about 33% at the end of May 2021, says the team.
When the third wave began to subside in late April, only about 5% of the population were fully vaccinated. The vaccine coverage was almost zero among those aged 0 to 69 years, with only hospital workers and people from other selected professions have been immunized.
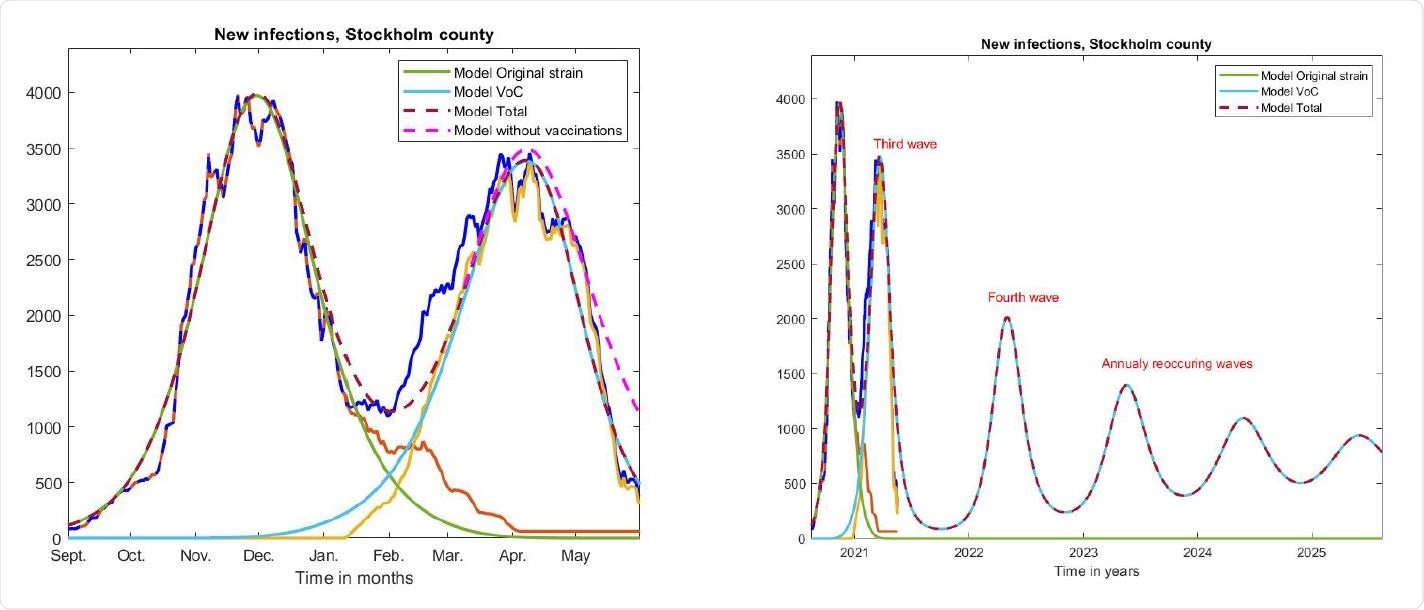
Left; same curves as in Figure 3 on a longer time-scale, along with curves produced by our model.
“Herd immunity” is the accepted scientific consensus
Carlsson and Soderberg-Naucler say that these figures would lead most scientists to conclude that NPIs and voluntary behavioral changes made the second wave bend downwards in early November and that public weariness and/or mutant viral strains caused the third wave. They would also assume that the third wave bent downwards due to renewed public compliance with recommendations in the face of the recent surge, adds the team.
“Indeed, this is the by now accepted scientific consensus among scholars studying the pandemic, which is sometimes called ‘herd-protection,’ and builds on the simple idea that when a major deadly epidemic hits, society reacts in a way that is impossible to predict mathematically,” writes the team.
“The pandemic response in Sweden challenges this interpretation”
However, the pandemic response in Sweden challenges this interpretation with Carlsson and Soderberg-Naucler now presenting an alternative explanation for the pattern of viral spread.
The team says experts have previously proposed that “pre-immunity” or immunological “dark matter” could underlie the unexpected trajectory of the COVID-19 pandemic.
However, failure to identify this dark matter together with various erroneous predictions involving pre-immunity led to the hypothesis being discarded.
“We believe that it is too early to discard the hypothesis that some sort of pre-immunity needs to be taken into account, in particular for accurate mathematical modeling,” said the researchers.
The team suggests that what looks like pre-immunity on a population level, could in fact be a consequence of large variability in individual-level susceptibility. Furthermore, this susceptibility may depend on innate immunity and cross-reactive protective immunity initiated by another virus or other factors.
Pre-immunity is a necessity for successful mathematical modeling
Carlsson and Soderberg-Naucler have now shown that mathematical models considering variable susceptibility to SARS-CoV-2 are equivalent to simpler models that incorporate pre-immunity.
“Pre-immunity is a necessity for successful mathematical modeling of the pandemic,” they say.
“We argue that this is the key factor that has protected Sweden from a much higher hospitalization rate and death toll, given the Swedish mitigation strategy, and that it helps to keep cases down to a much greater extent than predicted by traditional models for disease spread,” write the researchers.
However, “since cases can still go up if NPI’s are lifted, the term herd-immunity can be misleading… we call it herd-immunity under limited restrictions,” they add.
Vaccination is a must
The team emphasizes that this study is not suggesting that it is safe to lift NPI’s, but rather it implies that around 60% of the community could have some level of protection against SARS-CoV-2 under current NPIs.
Such protection could disappear due to emerging mutations and exposure to higher viral doses following the lifting of restrictions, say the researchers.
Furthermore, it is impossible to know if pre-immunity is present or not, they write.
“Based on this, it is our firm conclusion that the vaccination roll-out must continue with high participation to avoid both personal tragedies and COVID-19 becoming endemic.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources