SARS-CoV-2, the virus responsible for the COVID-19 pandemic, is highly transmissible, with nasal passages being the target of original infection. The nasal passage also shows the highest expression of ACE2, a protein that has been widely linked with increased susceptibility to COVID-19. Now, scientists from Japan have found that nasal inflammation can influence susceptibility to SARS-CoV-2. They also identified the use of short chain fatty acids as a potential COVID-19 management strategy.
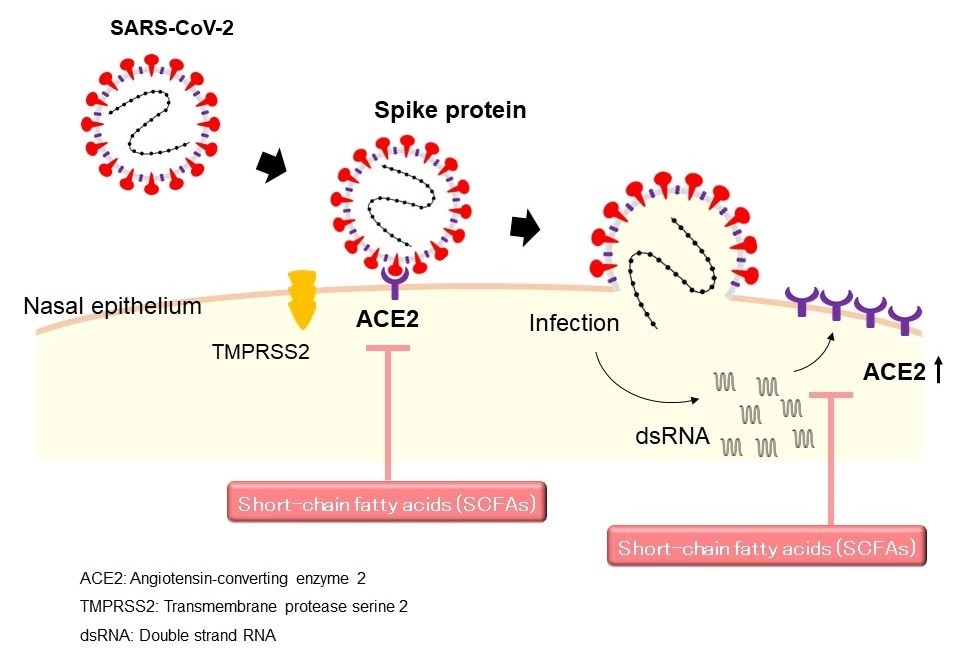
Image Credit: University of Fukui, Japan
Humans are no stranger to coronavirus (CoV) pandemics. Just like SARS-CoV-2 (the virus that causes COVID-19), another member of the coronavirus family--SARS-CoV--caused the severe acute respiratory syndrome (SARS) epidemic across parts of Asia in 2003. But, its spread was contained way faster than COVID-19. So, what makes SARS-CoV-2 so contagious?
Both SARS-CoV and SARS-CoV-2 viruses bear "spike proteins" which get inside our cells by binding to a protein called angiotensin-converting enzyme 2 (ACE2) that is found in our cells. However, the SARS-CoV-2 spike (S) protein has been found to have a higher binding affinity (10 to 20 times that of SARS-CoV) to ACE2, thus establishing a link between the pathogen and the protein.
Interestingly, recent studies have shown that patients with COVID-19 who have rhinosinusitis (i.e., inflammation of the nose) have a low risk of hospitalization. Moreover, the expression of ACE2 was reduced in patients with rhinosinusitis. Coincidentally, another study has shown that short-chain fatty acids (SCFAs), produced by bacteria in the gut have beneficial effects in allergy and viral infections. These separate findings prompted an investigation of the effect that SCFAs in the nasal cavity against SARS-CoV-2 infection by scientists from the University of Fukui, Japan, led by Dr. Tetsuji Takabayashi.
In a new study published in the American Journal of Rhinology & Allergy, the scientists attempted to understand the effect of SCFAs on ACE2 expression in the nasal passage, and the potential impact on COVID-19 infection.
This is the first report that short-chain fatty acids (SCFAs) effectively reduce the ACE2 levels in human airway epithelial cells."
Dr. Tetsuji Takabayashi, University of Fukui, Japan
To understand the status of ACE2 expression in patients with allergies, the researchers studied the levels of ACE2 in the inner lining of the nose in patients with seasonal allergic rhinitis induced by Japanese cedar pollen (SAR-JCP) and chronic rhinosinusitis (CRS). Using techniques like real time-PCR to quantify the expression of ACE2, the researchers found that there was no increase in ACE2 expression in in patients with SAR-JCP, whereas it was decreased in patients with CRS.
To better understand the effect of SCFAs on ACE2 expression, the researchers cultured nasal epithelial cells and exposed them to either SFCA and double-stranded RNA (similar to the nuclear material found in some viruses and known to enhance ACE2 expression). Upon examining the expression of ACE2, the researchers saw that the SFCAs had suppressed ACE2 expression in the presence of the RNA as well.
These results suggest that SFCAs has potential therapeutic applications against COVID-19.
The nasal mucosa exhibits the highest ACE2 expression among human organs and hence is a prominent target of original infection. Therefore, the development of strategies to downregulate ACE2 expression in nasal epithelial cells could reduce SARS-CoV-2 transmission and be useful as a novel therapeutic approach."
Dr. Tetsuji Takabayashi
The team's timely findings will certainly aid in our fight against COVID-19.
Source:
Journal reference:
Takabayashi, T., et al. (2021) Regulation of the Expression of SARS-CoV-2 Receptor Angiotensin-Converting Enzyme 2 in Nasal Mucosa. American Journal of Rhinology & Allergy. doi.org/10.1177/19458924211027798.