India continues to grapple with the coronavirus disease (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). To date, the country has reported over one million new cases for the past 28 days.
The country also saw increasing instances of COVID-19-associated mucormycosis (CAM), a systemic fungal infection caused by the Mucorales species. About 187 cases have been noted, prompting health officials to conduct rapid data collection and investigation.
The Mucorales species is the largest order of zygomycete fungi. Members of this order are sometimes called pin molds.
Researchers from the USA and India established an online registry of CAM cases in India and found that patients frequently received antibacterial drugs and zinc supplementation.
Their report was published in the U.S. Centers for Disease Control and Prevention (CDC) Emerging Infectious Diseases journal.
What is Coronavirus disease (COVID-19)–associated mucormycosis (CAM)?
Mucormycosis, also known as zygomycosis, is a severe but rare fungal infection caused by a group of fungi called mucormycetes. These fungi aren’t harmful to most people. However, for people who have weakened immune systems, breathing in mucormycete spores can cause an infection in the lungs or sinuses, which can spread to other parts of the body.
Several different types of fungi can cause mucormycosis. These fungi are called mucormycetes and belong to the scientific order Mucorales. The most common types that cause mucormycosis are the Rhizopus species and Mucor species. Other examples include Rhizomucor species, Syncephalastrum species, Cunninghamella bertholletiae, Apophysomyces, Lichtheimia (formerly Absidia), Saksenaea, and Rhizomucor.
Once the inhaled mucormycete spores take hold, they germinate to produce hyphae that can invade blood vessels and surrounding tissue, impeding blood flow that will cause tissue death. The sinuses and brain are common areas affected mainly by these fungi.
The symptoms include pain, headache, one-sided swelling of the face, blindness, fever, and black lesions where the necrotic tissue is located. Without early treatment and aggressive interventions, mucormycosis is fatal.
CAM cases in India
COVID-19 patients are treated with different drugs, including glucocorticoids, which can lead to secondary bacterial or fungal infections. The condition has emerged in 187 cases in India amid its fight against the SARS-CoV-2 Delta variant.
To determine the extent of CAM cases in India, the researchers established an online registry of cases. From there, they analyzed data from 65 patients diagnosed between April and June 2021, when the Delta variant predominated.
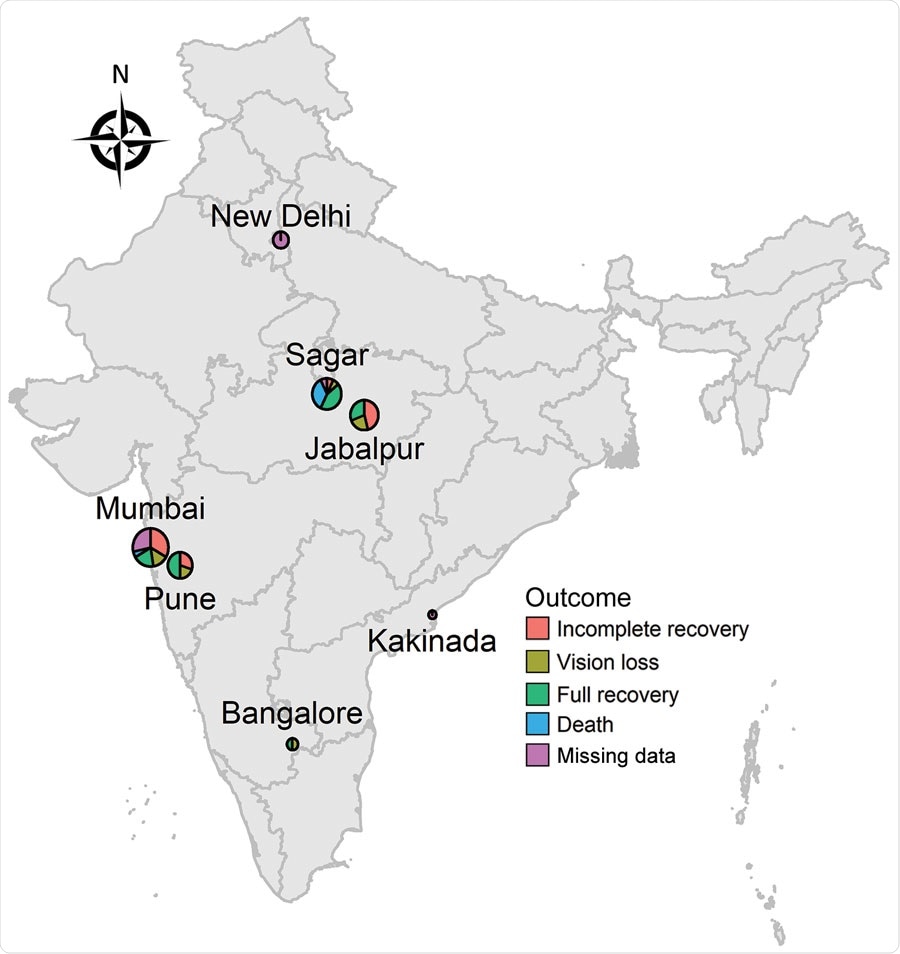
Geographic distribution of coronavirus disease-associated mucormycosis, India, 2021. Sizes of circles indicate the number of cases in that area. Use of the map recognized by the government of the United States does not endorse the territorial claims of any specific nation.
The researchers used the data collecting tool called Mycotic Infections in COVID-19 (MUNCO) in the study. It is valuable for doctors in settings where electronic medical records are rarely used in patient follow-up.
The team found that these patients were frequently given antibacterial drugs and zinc supplements. After a follow-up data for 53 patients, outcomes were defined as full recovery, incomplete recovery, including those with continued treatment at day 42, interrupted treatment, palatal perforation, stroke, paralysis, vision loss, or death.
The study findings showed that most patients are male and had diabetes. Among the study participants, only 3.1 percent had been taking long-term corticosteroids. However, most patients were treated with standard COVID-19 drugs, including remdesivir, corticosteroids, or both. Other treatments include zinc, ivermectin, favipravir, doxycycline, and azithromycin.
Among these patients, a majority reported fungal infections affecting the sinuses or eyes. The most common treatments are amphotericin B, Posaconazole, and surgery. Of the 53 patients with follow-up data at 42 days, 17 had an incomplete recovery, 20 patients fully recovered, 10 had vision loss, and six had died.
CAM causes
The researchers noted the findings in previous studies that diabetes and steroid use are risk factors that can increase the risk for CAM. Also, the team found frequent use of antibiotics in COVID-19 patients.
Zinc supplementation has also been reported. Overall, 57 percent of the patients received zinc supplements, perhaps due to the pathogenic fungi seize zinc from host tissues. Fungal cells must acquire zinc for proper development during their life cycle. On the other hand, zinc chelators can help inhibit the growth of some virulent fungi.
All these factors may increase the risk of developing CAM, which needs prompt treatment. The rapid, real-time collection of data using online registries of CAM cases can shed light on the disease and its potential treatments.
“In summary, our results show that online registries are a valuable tool to rapidly provide relevant data for real-time surveillance of emerging infections,” the team concluded in the study.