Scientists have claimed that the continual spread of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) virus can only be contained through rapid vaccination. SARS-CoV-2 is a positive-stranded RNA virus that has caused the coronavirus disease (2019) pandemic. Researchers worldwide worked at an unprecedented speed to develop vaccines and therapeutics to contain the ongoing pandemic. Several vaccines have received emergency use authorization (EUA) from various regulatory bodies, while others are undergoing clinical trials.
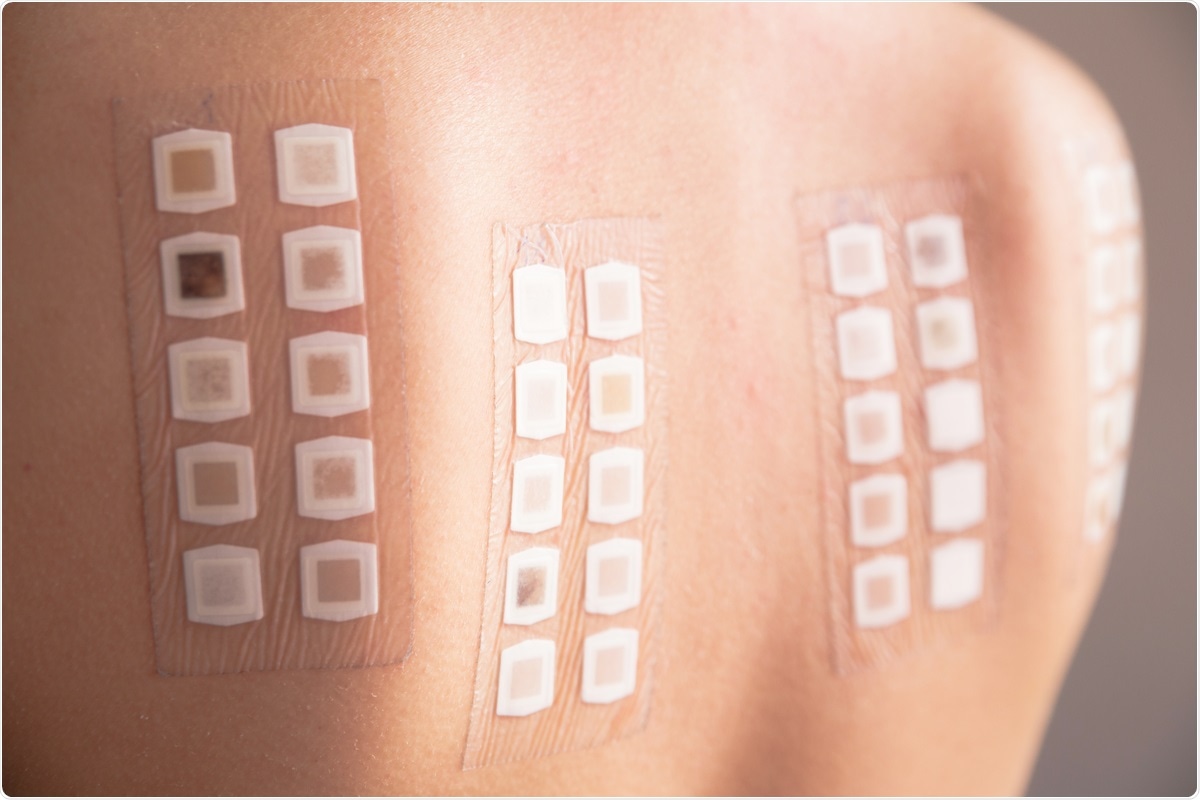 Study: Adverse reactions to BNT162b2 mRNA COVID-19 vaccine in medical staffs with a history of allergy. Image Credit: Neeila/ Shutterstock
Study: Adverse reactions to BNT162b2 mRNA COVID-19 vaccine in medical staffs with a history of allergy. Image Credit: Neeila/ Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The BNT162b2 vaccine, developed by Pfizer-BioNTech, was the first available mRNA vaccine in Japan in February 2021. According to the clinical trials, BNT162b2 was 95% effective in preventing symptomatic COVID-19 infection in vaccinated individuals. Although the healthcare workers (HCW) were the first to be vaccinated, the increase in the availability of many other approved vaccines enhanced the rate of vaccination among the general population.
COVID-19 vaccines and adverse reactions
Although vaccination is the most effective means to manage SARS-CoV-2 infection, all the approved vaccines have shown certain adverse reactions. The most common adverse reactions are pain at the site of vaccination, fever, and some allergic symptoms. However, a more serious adverse reaction is also associated with vaccination, the development of anaphylaxis, a life-threatening condition.
As COVID-19 vaccines are new, there are many unknown factors. For instance, it is unknown if an individual will develop an allergy or severe anaphylaxis after being vaccinated. It has been extremely difficult to determine if an individual with allergies should be vaccinated. This is because, in the clinical trials, which evaluate the safety of a vaccine, individuals with a history of allergy were excluded. To date, a limited number of studies are available that assess the safety of COVID-19 vaccines in individuals with a history of allergies.
Evaluation of the safety of the BNT162b2 vaccine for individuals with allergies
Scientists have addressed the gap in the research regarding the adverse reactions to the COVID-19 vaccine among individuals with allergies. They published their findings on the medRxiv* preprint server. The current study was conducted at Yamagata University Hospital, Japan, where the BNT162b2 mRNA COVID-19 vaccine was administered to hospital staff and medical students between March 3, 2021, and August 27, 2021.
The authors of this study conducted a survey to determine (a) if any of the vaccinated health care staff and medical students had a history of allergy and (b) adverse reactions after immunization among them. Subsequently, researchers analyzed the data and verified the safety of the COVID-19 vaccine among this group.
In this study, researchers circulated the questionnaire to their subjects after receiving the first and second doses of the vaccine. The participants were asked if they had a history of allergies, and in case of any, the nature of the allergy was asked to be reported. Further, they were asked if they experienced any adverse reactions post-immunization and, if any, the duration and all details associated with it.
Researchers obtained responses from 1586 participants after the first vaccination and 1306 participants after the second dose of the BNT162b2 vaccine. After analyzing the data, scientists revealed that some common adverse reactions such as pain and swelling at the vaccination site, fever, fatigue, headache, nausea, chills, arthralgia, and muscle pain outside the vaccination site prevailed. Typically, the frequency and severity of the most adverse reactions were found after the second vaccination dose than the first. Also, interestingly, this study revealed that females and younger individuals experienced adverse reactions at a higher rate than males and the elderly.
The present study reported that the subjects with a history of allergies experienced some adverse reactions with higher severity, and the duration of symptoms lasted for a longer period compared to subjects without any allergies. This result agrees with a previous study that reported COVID-19 vaccination of hospital staff showed a higher frequency of adverse reactions in the presence of allergy.
Most importantly, even though some participants had to visit an emergency room for treatment after receiving the first or second dose of the vaccine, none experienced anaphylaxis. This result indicated that no serious life-threatening allergic reactions occurred among the subjects, despite having a history of allergy, post the BNT162b2 vaccination.
Conclusion
This study has several limitations. For instance, this survey was an internet-based questionnaire, and all the symptoms were self-reported. Thereby, it is not clear if the diagnosis of the allergic reactions was correct. Also, very few subjects had a history of anaphylaxis or adverse allergic reaction, so the statistical reliability of the data was not strong. However, the authors of this study recommended vaccination for individuals with a history of allergy as no serious adverse reaction surfaced among the subjects after immunization.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Inoue, S. et al. (2021) "Adverse reactions to BNT162b2 mRNA COVID-19 vaccine in medical staffs with a history of allergy". medRxiv. doi.org/10.1016/j.resinv.2021.11.007.
- Peer reviewed and published scientific report.
Inoue, Sumito, Akira Igarashi, Keita Morikane, Osamu Hachiya, Masafumi Watanabe, Seiji Kakehata, Shinya Sato, and Yoshiyuki Ueno. 2022. “Adverse Reactions to BNT162b2 MRNA COVID-19 Vaccine in Medical Staff with a History of Allergy.” Respiratory Investigation 60 (2): 248–55. https://www.sciencedirect.com/science/article/pii/S2212534521001957.