As of September 20, 2021, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is the virus responsible for the coronavirus disease 2019 (COVID-19), has infected over 229 million individuals and caused over 4.69 million deaths globally. COVID-19 vaccinations across the world have rendered some protection against SARS-CoV-2.
Non-pharmaceutical interventions including lockdowns, physical/social distancing, closure of all public establishments, and the wearing of masks/shields have helped significantly from the start of the pandemic to contain the spread of SARS-CoV-2. Policymakers and researchers are assessing the ability of these risk mitigation strategies to provide a safer and healthier space.
 Study: Social Capital Dimensions are Differentially Associated with COVID-19 Vaccinations, Masks, and Physical Distancing. Image Credit: Zubada / Shutterstock.com
Study: Social Capital Dimensions are Differentially Associated with COVID-19 Vaccinations, Masks, and Physical Distancing. Image Credit: Zubada / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
What is social capital?
In this context, assessing the social capital of a community reflects the value of a community structure. This approach is widely used to understand social determinants of public health.
Social capital is measured using different social elements from different aspects of the community. For example, social capital stemming from family support has been associated with better mental health, better mechanisms for coping with stress, and lower suicide rates.
“To better reflect the nature of communities, social capital has further been defined as the quality of the relationship among community members, which is represented in trust and reciprocal aid that derive mutual benefits to all parties.”
A new study
A recent study published on the preprint server medRxiv* examines the relationship among public health behaviors during the COVID-19 pandemic including vaccination, face masking, and physical distancing, and social capital indices in counties in the United States. The researchers of this study found the social capital index and its subindices differentially correlate with different public health behaviors.
Despite the recommendations to be adopted during the pandemic to limit viral transmission and protect self and others, some communities found it difficult to isolate and eliminate social gatherings. Comparatively, other communities abided uniformly to the new recommendations and acted responsibly.
Because communities are structured in a way that impacts individuals’ ability to adopt new behaviors and follow public health recommendations, the researchers of the current study explored the association between different capital facets and public health behaviors during the COVID-19 pandemic at the county-level in the United States. Social capital in the U.S. is operationalized and measured on the county and the state levels.
The researchers used publicly available vaccination data as of June 2021, face masking data in July 2020, and mobility data from mobile phones movements from the end of March 2020. They conducted correlation analyses with county-level social capital index and its subindices, of which included family unity, community health, institutional health, and collective efficacy.
This information was obtained from the Social Capital Project by the United States Senate. According to the Social Capital Project, family unity considers the structure of families in terms of marriage and children, whereas community health considers participation in civic life such as involvement in volunteering and religious groups.
The third classification of institutional health considers confidence in media/corporations/schools, as well as participation in institutions such as elections and census. Finally, collective efficacy is the converse of social disorganization, operationalized via violent crime rates.
This study estimated the effects of social capital on public health behaviors related to the COVID-19 pandemic using a list of variables in the analysis with descriptive statistics. The variables included social capital, family unity, community health, institutional health, collective efficacy, full vaccination or hesitancy (as of June 2021), wearing masks or never (June 2020), mobility index (Week of 23 March 2020), retail and recreation, and residential. The researchers assessed the bivariate relationships between each social capital index and public health behavior using standardized linear regression.
Study results
“Each public behavior affected by different social capital facets resembles a defensive layer against the spread of COVID-19,” observed the researchers in the study.
The researchers found that vaccination mostly associates significantly with institutional health. To this end, counties with high institutional health exhibited an increased rate of vaccination. Thus, trusting institutions promote more vaccinations.
Most counties where individuals reported wearing masks were associated with community health.
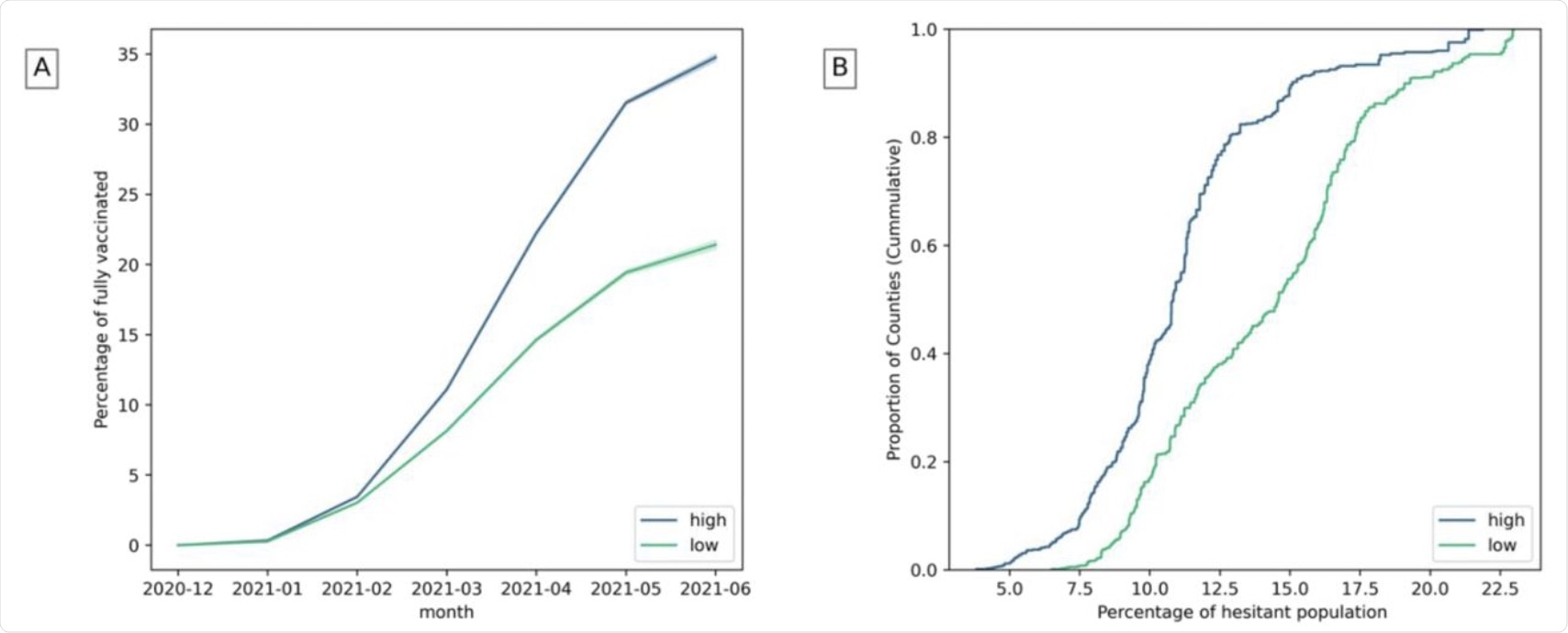 A) Fully vaccinated population over time in counties with high and low institutional health. B) Estimated hesitant population in counties with high and low institutional health. (The highest and lowest 25% of counties are considered).
A) Fully vaccinated population over time in counties with high and low institutional health. B) Estimated hesitant population in counties with high and low institutional health. (The highest and lowest 25% of counties are considered).
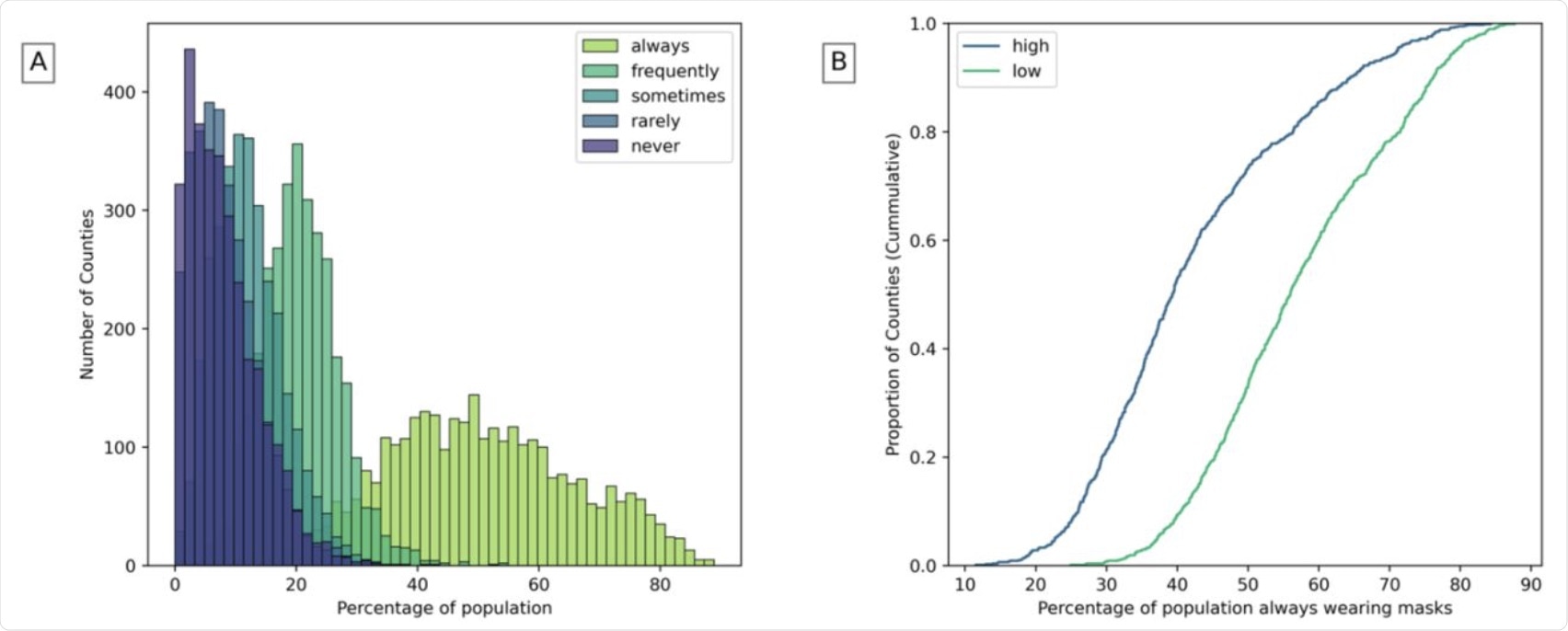 A) Population that wears masks in counties. B) Population that always wears masks in counties with high and low community health (The highest and lowest 25% of counties are considered).
A) Population that wears masks in counties. B) Population that always wears masks in counties with high and low community health (The highest and lowest 25% of counties are considered).
Reduced mobility associates mostly with higher overall social capital and secondly with community health, while increased residential mobility associates mostly with higher family unity. Therefore, communities engaged in more civic life were more responsible and reduced their mobility.
Furthermore, stronger family ties were associated with an increased likelihood of people remaining home. Better social capital and institutional health also decreased recreational visits.
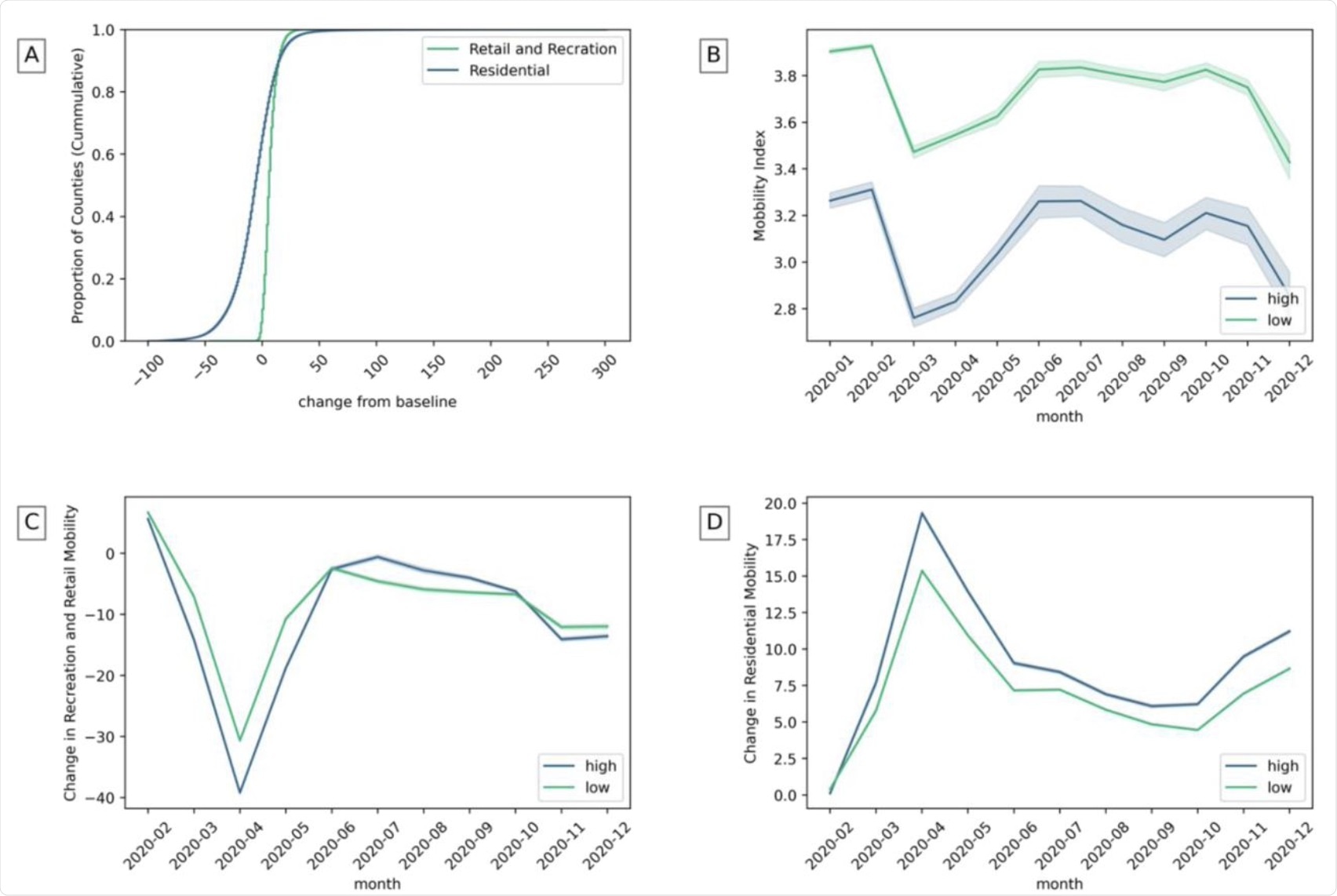 A) The change of recreation and residential mobility in counties. B) Mobility index in counties with high and low community health. C) Recreation and retail mobility in counties with high and low institutional health. D) Residential mobility with high and low family unity. (The highest and lowest 25% of counties are considered).
A) The change of recreation and residential mobility in counties. B) Mobility index in counties with high and low community health. C) Recreation and retail mobility in counties with high and low institutional health. D) Residential mobility with high and low family unity. (The highest and lowest 25% of counties are considered).
“As such, our results suggest that differential facets of social capital imply a Swiss cheese model of pandemic control planning where, e.g., institutional health and community health, provide partially overlapping behavioral benefits.”
Study takeaways
In conclusion, this study shows that facets of social capital are differently associated with behavioral responses to the COVID-19 pandemic. The results observed here emphasize that social capital and its subindices are essential in explaining differences in public
behaviors during health crises which may help determine policies in local communities. Notably, communities with lower social capital need more effort to help individuals adopt new protective behaviors.
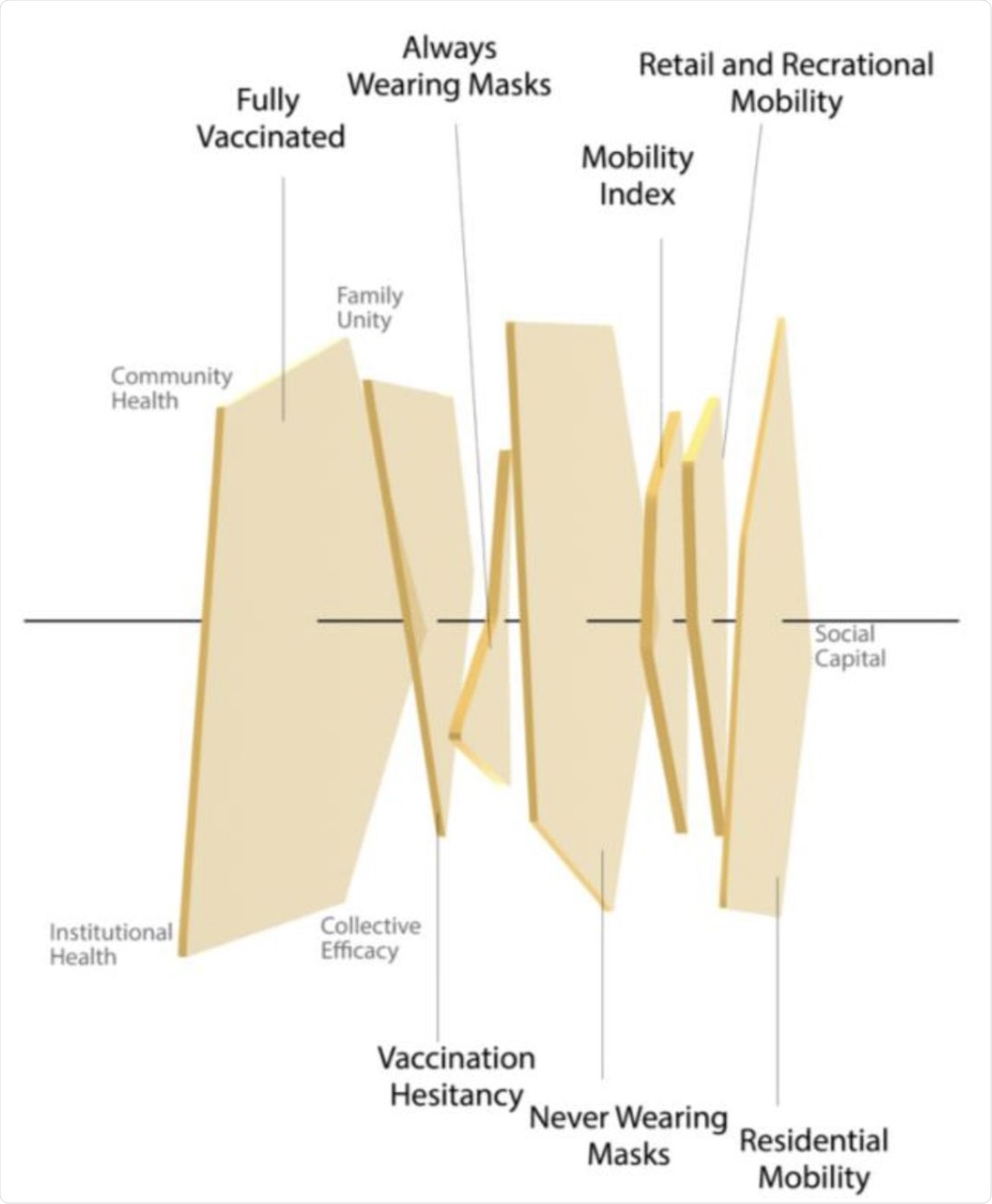 A Swiss cheese model for social capital, with pentagons representing the five social capital indices’ impact on social behaviors.
A Swiss cheese model for social capital, with pentagons representing the five social capital indices’ impact on social behaviors.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources