Severe acute respiratory syndrome coronavirus (SARS-CoV-2) is a novel virus that causes coronavirus disease (COVID-19). Early detection of Immunoglobulin G (IgG) against SARS-CoV-2 spike proteins in COVID-19 patients has been reported, which is not typically observed in other infections. It has been suggested that the early response may be the result of prior exposure to seasonal human coronaviruses (hCoV), which are known to be prevalent in the population. Due to these prior exposures, this recall response may contribute to the enhanced immune response observed in COVID-19 patients.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Non-hospitalized COVID-19 convalescent individuals exhibited a wide range of symptoms
The history of symptoms displayed by convalescent SARS-CoV-2 individuals and the severity of their symptoms was investigated in 48 patients from New York City who had SARS-CoV-2 infection during the first wave of the pandemic and were not hospitalized.
The study was conducted on subjects who tested positive for SARS-CoV-2 and who were recovering from infection. Subjects who tested negative for SARS-CoV-2 were treated as negative controls. The blood samples for analysis were collected from convalescent subjects at 43 days after symptom onset to ensure sufficient levels of anti-SARS-CoV-2 IgG were present for analysis.
The severity and the duration of symptoms were assessed in the convalescent donors, and average severity score was calculated for each symptom, and a composite severity score was also determined for each study subject.
It was found that the convalescent donors exhibited a range of mild to severe symptoms, with the most common symptoms being cough, headache, muscle pain and fatigue. Fatigue, muscle pain and diarrhea got the highest average symptom severity scores. Nausea and vomiting were identified as the least frequently occurring symptoms.
With regard to a composite severity score, convalescent donors were classified as having mild symptoms (MILD) if their score was below 45 and as having severe symptoms (SEVERE) if they scored more than 45.
The common symptoms experienced by convalescent subjects with severe composite scores include high fevers more than 101°C that extended for more than a week, muscle pain, difficulty breathing and headache.
In addition, difficulty in breathing and diarrhea were experienced by more subjects in the SEVERE group when compared to the MILD group. With other symptoms, the groups differed by the severity of occurrence.
Increased levels of anti-spike IgG antibodies are associated with disease severity in non-hospitalized COVID-19 convalescent individuals
The study attempted to estimate IgG levels in convalescent donors against SARS-CoV-2 spike protein to evaluate the levels of humoral immune response in these subjects that were associated with mild and severe COVID-19 infection.
It was observed that anti-spike IgG levels were significantly increased in convalescent donors when compared to negative controls. The levels of anti-spike IgG levels also correlated with the composite severity scores with high levels of anti-spike IgG corresponding to high severity scores and vice versa.
Non-neutralizing effector responses are also associated with IgG, which is facilitated by antigen recognition on the surface of host cells. This was investigated by using cell-based assays assessing IgG binding to SARS-CoV-2 spike, which also showed a positive correlation between levels of anti-spike IgG and disease severity.
Multivariable analysis identifies that mild and more severe COVID19 is differentiated by distinct humoral immune profiles. (A) Scatter matrix chart summarizes the Spearman’s correlation (upper) and the scatter plots (lower) between all analyzed variables using the entire cohort (n=28). The Spearman’s r values are shown inside the colored squares and the scale of blue-to-red color indicates a negative-to1584 positive correlation. The small bar graphs (diagonal) represent the distribution of data for each variable (B) Biplot shows the principal component analysis (PCA) depicting the mild-scored (n=13) and more severe-scored (n=15) COVID-19 patients, according to their severity scores (C) The contribution of each variable to PCA for dimension 1 and 2 is represented by bars, and its threshold is indicated as a red dotted line. (D,E) Polar plots show the different profiles of humoral response for mild and more severe groups. Each bar in the plot represents the mean of z-scores for each variable.
Increased levels of FcγR activation induced by anti-spike IgG antibodies are associated with disease severity in non-hospitalized COVID-19 convalescent individuals
Earlier studies have shown that levels of both anti-spike IgG and pro-inflammatory cytokines are increased in severe SARS-CoV-2 infections that require hospitalization. This effect may be due to IgG aggravating SARS-CoV-2 infection through FcγR associated antibody-dependent enhancement (ADE).
ADE is the phenomenon where viruses bind to antibodies performing sub-optimally and gain entry into host cells through FcγR and subsequently replicate, resulting in worsening infection.
The present study assessed the levels of IgG stimulated FcγR-signalling in convalescent study subjects. Specifically, the levels of FcγR2a and FcγR3a receptors were examined in this study as these receptors are known to mediate Ab-dependent cellular-cytotoxicity (ADCC), Ab-dependent cellular phagocytosis (ADCP) and activate pro-inflammatory cytokines.
A significant positive correlation between levels of FcγR2a and FcγR3a activation and severity scores were observed. The intensity of this effect was more in convalescent subjects classified as SEVERE. IgG from SEVERE subjects significantly increased levels of both FcγR2a and FcγR3a activation. However, IgG from MILD subjects increased FcγR2a activation alone.
The levels of anti-spike IgG and FcγR2a and FcγR3a activation also showed a significant positive correlation. In convalescent donors, a strong positive correlation exists between FcγR2a and FcγR3a signaling, COVID-19 severity and levels of anti-spike IgG.
Seasonal hCoV recall responses in non-hospitalized COVID-19 convalescent individuals
Unlike typical instances where IgG elicited response against antigens takes several days to manifest, increased levels of IgG have been detected in less than 4 days of SARS-CoV-2 infection.
Seasonal human alpha and beta coronaviruses are prevalent in the population. It is common for 4-27% of people to test positive for any hCoV at any given instance. There is high sequence similarity between the spike protein of commonly occurring coronaviruses and SARS-CoV-2.
The study's scientists hypothesized that humoral immune responses that were elicited against common coronaviruses may have enhanced the IgG response towards SARS-CoV-2 spike protein in infected patients.
They investigated this recall response further by assessing if IgG from convalescent donors exhibits cross-reactivity and binds to spike proteins from common hCoV and SARS-CoV-1.
It was found that anti-spike IgG from SARS-CoV-2 convalescent donors significantly recognized the spike protein from beta coronavirus and SARS-CoV-1 but not the ones from alpha coronavirus. The spike proteins from SEVERE convalescent donors exhibited higher levels of cross-reactivity than those from MILD donors.
Immunodominant regions are regions in the antigenic determinants that are easily recognized by the immune system and significantly contribute to the specificity of the antibody produced.
Recent studies have identified immunodominant regions in the spike protein that also share sequence similarities with common coronaviruses like the beta coronavirus OC43. IgG recognition of these immunodominant regions may be due to recall responses from earlier infections with common coronaviruses.
The study investigated anti-spike IgG targeting against peptides containing immunodominant regions that are both conserved and non-conserved between SARS-CoV-2 and the beta coronavirus OC4.
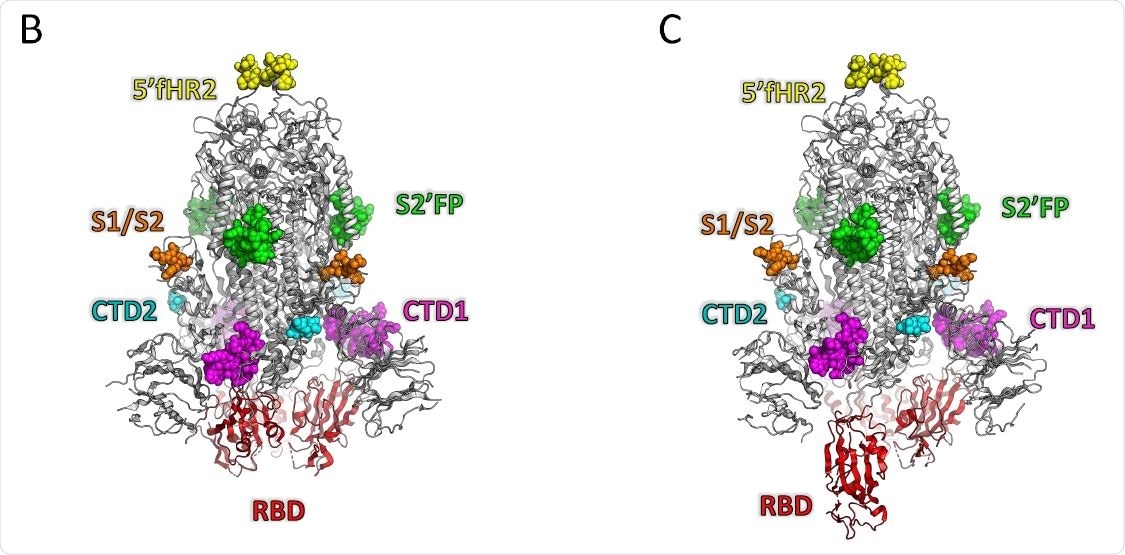
A significant positive correlation exists between anti-spike IgG binding and disease severity in the case of S2' cleavage fusion protein (S2'FP) region, which is highly conserved between SARS-CoV-2 and beta coronavirus OC4 and the c-terminal domain 1 (CTD1) region, which is a non-conserved region.
On the other hand, a negative correlation exists between anti-spike IgG binding and disease severity in the case of the receptor-binding domain (RBD), highly conserved heptad repeat 2 (HR2) domain and a region upstream of HR2 called 5' flank HR2 (5'fHR2). Importantly there was more anti-spike IgG binding to HR2 and RBD in the case of MILD convalescent donors when compared to SEVERE donors.
Association between ant-spike IgG levels, beta coronavirus cross-reactivity, IgG immunodominant region targeting, FcγR signaling and non-hospitalized COVID-19 severity
A multivariate analysis was performed to understand the association of all parameters studied, including ant-spike IgG levels, beta coronavirus cross-reactivity and FcγR signaling.
When all convalescent donors were compared, SEVERE convalescent donors showed higher anti-SARS CoV-2 spike IgG levels, cross-reactivity to beta coronaviruses, pro-inflammatory FcγR activation anti-spike IgG targeting the S2'FP region and CTD1 regions. Higher severity scores inversely correlated with IgG targeting RBD and HR2 regions. Beta coronavirus cross-reactivity is highly correlated with levels of IgG targeting the immunodominant regions. FcγR2a and FcγR3a activation were also positively correlated with beta coronavirus cross reactivity. When compared to FcγR3a, FcγR2a activation was highly correlated with levels of IgG targeting the CTD1 and S2'FP regions.
Prior exposure to hCoV influences the specific regions in the SARS-CoV-2 spike protein that are targeted by IgG. The IgG response levels and disease severity highly depend on the specific regions that are targeted.
Implications of the present study
- Previous exposure to seasonal coronaviruses especially beta coronavirus and the immunological response to the exposure determines and predicts the severity of COVID-19 infections.
- An anti-HR2 dominant IgG antibody profile is associated with a protective recall response, while an anti- S2'FP dominant IgG antibody profile is associated with a recall response that can lead to severe disease. Anti-RBD dominant IgG profile is also protective and is a novel response.
- Assessing the antibody profiles of patients will help in early interventions to reduce disease severity and prevent acute respiratory distress syndrome (ARDS).
- The antibody profiles induced by vaccines should also be assessed. Current mRNA vaccines predominantly induce anti-RBD-specific antibodies after the second dose ensuring a protective effect. The antibody profiles induced by various vaccines will help determine their effectiveness against SARS-CoV-2.
- It may be necessary to assess the ratio of IgG targeting RBD and other immunodominant regions to determine the duration of immune protection and the number of breakthrough infections. Individuals with poor responses to vaccines may be recommended vaccines that may target the RBD or HR2 regions to improve their protection against SARS-CoV-2. HR2 region may prove to be an effective target for hCoV treatment and vaccine development.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Humoral immune responses against seasonal coronaviruses predict efficiency of SARS-CoV-2 spike targeting, FcγR activation, and corresponding COVID-19 disease severity Jose L. Garrido, Matias Medina, Felipe Bravo, Sarah McGee, Francisco Fuentes, Mario Calvo, James W. Bowman, Christopher D. Bahl, Maria Inés Barría, Rebecca A. Brachman, Raymond A. Alvarez, bioRxiv, 2021.09.14.460338; doi: https://doi.org/10.1101/2021.09.14.460338, https://www.biorxiv.org/content/10.1101/2021.09.14.460338v1
- Peer reviewed and published scientific report.
Smith, Kelly D., David K. Prince, Kammi J. Henriksen, Roberto F. Nicosia, Charles E. Alpers, and Shreeram Akilesh. 2022. “Digital Spatial Profiling of Collapsing Glomerulopathy.” Kidney International 101 (5): 1017–26. https://doi.org/10.1016/j.kint.2022.01.033.