Coronavirus disease 2019 (COVID-19) pandemic that spread worldwide in 2019 posed the greatest threat to at-risk groups, such as the elderly, those with respiratory disorders, and chemotherapy patients with compromised immune systems. Most of these people isolated themselves completely in line with 'shielding' advice.
Now that COVID-19 is slowly being brought under control by mass vaccination programs, monoclonal antibody treatment and repurposed drugs, restrictions are beginning to ease. However, there are still worries over the high risk of severe illness in the elderly, especially as variants of concern (VOCs) become more common.
The Delta variant, in particular, is now the most commonly seen form of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and previous studies have shown that pre-existing immunity, both natural and vaccine-induced, is significantly less effective against this strain.
In order to qualify the risk posed to the elderly, researchers from MUSE University in France began to investigate data from nursing homes that had faced outbreaks from variants of concern. Their work can be found on the medRxiv* preprint server while awaiting peer review.
The researchers examined data from two nursing homes that had suffered outbreaks of the Delta variant, as well as previous outbreaks of COVID-19. In the first nursing home (NH1), an initial COVID-19 outbreak was seen in December 2020. Both vaccination doses were provided to the residents in March and May of 2021.
A second outbreak, in this case, the Delta variant, occurred in July and August of 2021. The second nursing home (NH2) showed a similar story, with an outbreak over April-June 2020, two vaccines doses over February and March 2021, and a Delta variant outbreak in August 2021.
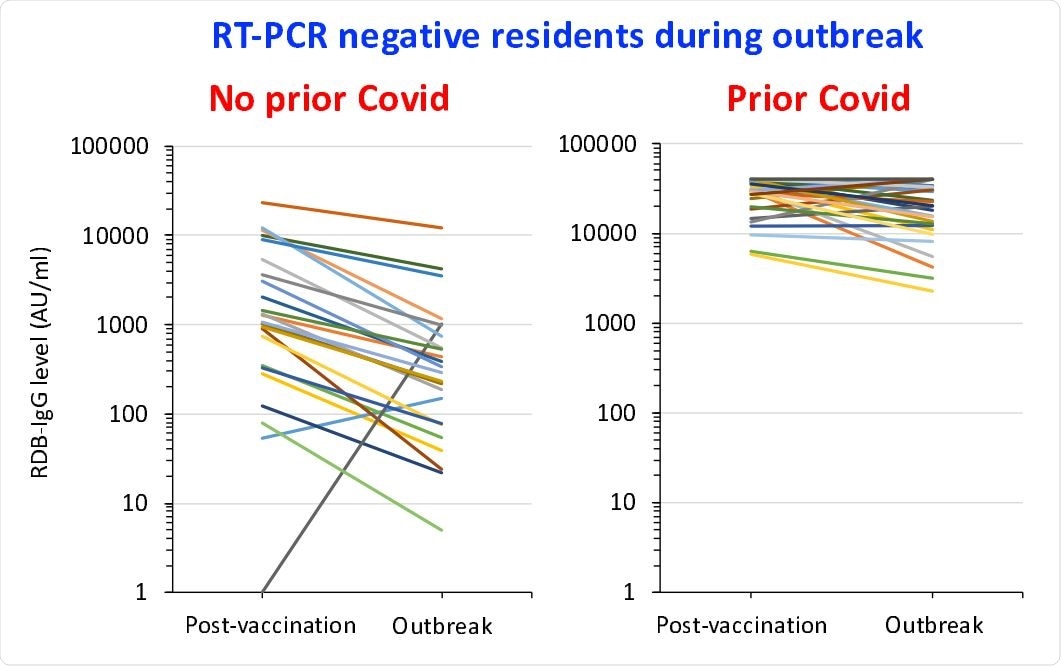
Change with time in RDB-IgG levels in residents with a negative RT-PCR during the outbreak: measures taken both 6 weeks after the second vaccine dose and during the outbreak
Infection with SARS-CoV-2 was confirmed with RT-PCR. To determine whether vaccinated and previously infected individuals were more protected than those who had not been, the researchers examined the levels of IgG antibodies targeting the receptor-binding domain (RBD) of the S1 subunit of the spike protein of SARS-CoV-2.
The RBD is the common target for most vaccines and most antibody treatments, as the RBD is essential to the pathogenicity of the virus. It binds to angiotensin-converting enzyme 2 (ACE2) in order to allow viral cell entry as well as the N-terminal domain of the S2 subunit to begin membrane fusion.
The levels of anti-RBD antibodies were measured 6 weeks after the second vaccination and again during the Delta variant outbreak.
One hundred fifty-one residents between the ages of 58 and 101 were examined, including 104 females and 47 males. Eleven residents did not have outcomes that were evaluable. Forty-four residents had previously had COVID-19. One of these residents developed a Delta-strain infection during the outbreak, and an additional 55 non-previously convalescent individuals developed a Delta variant infection.
In both those who had and had not previously been infected, there was a significant reduction in anti-RBD IgG antibodies in the time between the vaccine and the outbreak, with a 27.5% and 69.6% reduction, respectively. Anti-RBD antibodies were significantly higher in those who had previously been infected.
As only one resident who had been previously infected and vaccinated was also infected by the Delta strain outbreak, the authors consider prior infection and vaccination to be significantly effective in preventing further outbreaks of the disease.
Unfortunately, there were also a large amount of double-vaccinated individuals who still became infected with SARS-CoV-2. This illustrates the level of immune evasion the Delta variant is capable of and should inform public health decisions in the future, especially regarding vulnerable individuals like the elderly.
This holds even more true for nursing home patients, as the collection of vulnerable individuals clustered closely together could allow for rapid outbreaks to spread quickly between patients.
These findings are supported by previous studies showing anti-RBD antibody levels rapidly deplete in vaccinated individuals, as well as multiple cases of Delta variant infection in fully vaccinated individuals.
Luckily, other studies also show that despite infection of vaccinated individuals being possible, the infections usually are far less severe and result in far fewer deaths.
The authors also highly support that a booster dose should be offered to those at risk in order to prevent anti-RBD IgG levels from decaying to the point where transmission is possible.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Blain, H, et al., (2021) Prior Covid-19 and high RBD-IgG levels correlate with protection against VOC-δ SARS-CoV-2 infection in vaccinated nursing home residents. medRxiv preprint server. doi: https://doi.org/10.1101/2021.09.21.21263880, https://www.medrxiv.org/content/10.1101/2021.09.21.21263880v1
- Peer reviewed and published scientific report.
Blain, Hubert, Edouard Tuaillon, Lucie Gamon, Amandine Pisoni, Stéphanie Miot, Valentin Delpui, Nejm Si‐Mohamed, et al. 2022. “Receptor Binding Domain‐IgG Levels Correlate with Protection in Residents Facing SARS‐CoV‐2 B.1.1.7 Outbreaks.” Allergy 77 (6): 1885–94. https://doi.org/10.1111/all.15142. https://onlinelibrary.wiley.com/doi/10.1111/all.15142.