Researchers in Australia have reported that pregnant women in Melbourne were more likely to have a preterm stillbirth during the period when coronavirus disease 2019 (COVID-19) lockdown restrictions were imposed on the city, than they were during the corresponding period one and two years prior.
The retrospective study conducted across twelve public maternity hospitals in Melbourne found that in the absence of high COVID-19 prevalence, rates of preterm stillbirth were significantly higher during the lockdown period of March 23rd, 2020, to March 14th, 2021, compared with the two previous years.
Lisa Hui from The University of Melbourne and colleagues say that further research is needed to understand whether this increase was related to changes in health service access and utilization, altered maternal pathophysiology, or other social and environmental factors.
A pre-print version of the research paper is available on the medRxiv* server, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Melbourne experienced a unique set of circumstances
The COVID-19 pandemic has been associated with a worsening of perinatal outcomes globally due to a combination of maternal COVID-19, changes in maternity care, and overloaded health services.
In 2020, the city of Melbourne endured a prolonged period of fluctuating lockdown restrictions between March 23rd, 2020, and March 14th, 2021.
During the strictest lockdown period in mid-2020, people were restricted from leaving their homes for anything other than essential work, caring for dependents and obtaining medical care or essential foods and services.
Multiple changes were made to pregnancy care to help minimize the anticipated strain on health services and to reduce infection risk. Such changes included a rapid transition to “telehealth,” increased intervals between in-person visits, reduced face-to-face appointment time, and modifications to gestational diabetes screening and fetal growth monitoring.
During this lockdown period, there were relatively few maternal COVID-19 infections in Melbourne (less than 100 in 2020), and no associated maternal or perinatal deaths were recorded.
“This meant that metropolitan Melbourne experienced a unique set of circumstances not seen in other high-income countries: a prolonged period of significant social restrictions and major changes to antenatal care, without an associated high burden of COVID-19 infections,” writes Hui and colleagues.
In mid-2020, all twelve public maternity hospitals in Melbourne formed the Collaborative Maternity and Newborn Dashboard (CoMaND) to internally monitor the effects of the COVID-19 on clinical quality indicators.
What did the current study involve?
Hui and colleagues used perinatal data collected for CoMaND to compare stillbirth and preterm birth rates between women exposed and unexposed to lockdown restrictions during pregnancy.
The team collected data on all singleton births without congenital anomalies from 24 weeks’ gestation across all twelve maternity services from 1st January 2018 to 31st March 2021.
The lockdown-exposed cohort included all women for whom weeks 20 to 40 of gestation would have occurred between March 23rd, 2020, and March 14th, 2021. The control cohort included all pregnancies in the corresponding period one and two years prior. The lockdown-exposed cohort comprised 24,017 births and the control cohort comprised a total of 50,017 births.
What did the study find?
The rate of preterm stillbirth was significantly higher in the lockdown-exposed group than in the control group, at 0.26% vs. 0.18%.
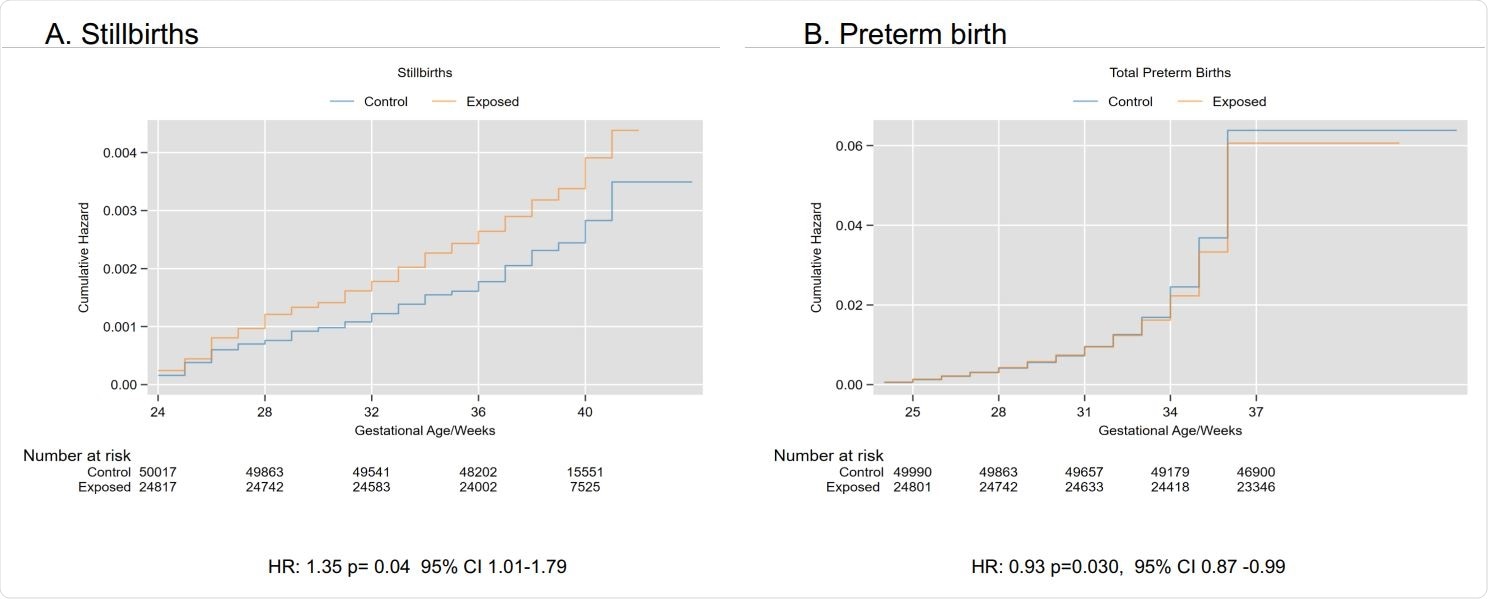
Stillbirth hazard ratio, CI, confidence interval; HR, hazard ratio
There was also a significant reduction in preterm births at less than 37 weeks gestation, at 5.93% versus 6.23%. This was largely mediated by a reduction in iatrogenic (induced or cesarian) preterm live births, at 3.01% versus 3.27%, including those initiated due to suspected fetal compromise (1.25% vs. 1.51%).
There was no significant difference in the spontaneous preterm birth rate between the exposed and control groups, at 2.69% versus 2.82%.
What did the researchers conclude?
The researchers say the study suggests that lockdown restrictions have significant impacts on perinatal outcomes, independent of the effect of COVID-19 disease.
“Our study shows that pregnant women exposed to lockdown in a high-income setting were less likely to have an iatrogenic preterm birth for suspected fetal compromise but more likely to have a preterm stillbirth,” they write.
Hui and colleagues suggest that the increase in stillbirth might be due to a maternal reluctance to present to hospital for decreased fetal movements or other medical or obstetrics concerns, rather than institution-specific barriers to in-person care.
The team advises that health services, consumers, practitioners, and policymakers must consider the consequences of the pandemic response on maternity care as part of continuing to navigate the second year of the pandemic.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Increase in preterm stillbirths and reduction in iatrogenic preterm births for fetal compromise: a multi-centre cohort study of COVID-19 lockdown effects in Melbourne, Australia. medRxiv, 2021. doi: https://doi.org/10.1101/2021.10.04.21264500, https://www.medrxiv.org/content/10.1101/2021.10.04.21264500v1
- Peer reviewed and published scientific report.
Hui, Lisa, Melvin Barrientos Marzan, Stephanie Potenza, Daniel L. Rolnik, Natasha Pritchard, Joanne M. Said, Kirsten R. Palmer, et al. 2022. “Increase in Preterm Stillbirths in Association with Reduction in Iatrogenic Preterm Births during COVID-19 Lockdown in Australia: A Multicenter Cohort Study.” American Journal of Obstetrics and Gynecology, April, S0002-9378(22)003015. https://doi.org/10.1016/j.ajog.2022.04.022. https://www.ajog.org/article/S0002-9378(22)00301-5/fulltext.