Drugs effective against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) normally work by either reducing the rate at which the virus replicates or reducing the damaging inflammation the disease causes.
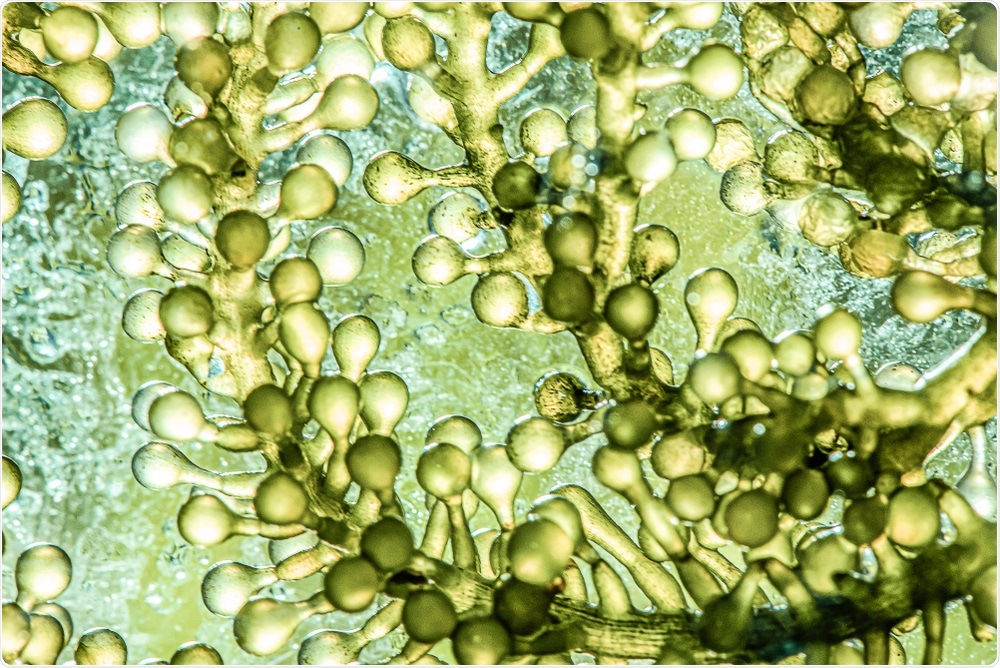 Study: Bioprospecting of microalgae metabolites against cytokine storm syndrome during COVID-19. Image Credit: Chokniti Khongchum / Shutterstock.com
Study: Bioprospecting of microalgae metabolites against cytokine storm syndrome during COVID-19. Image Credit: Chokniti Khongchum / Shutterstock.com
Background
Remdesivir, a drug that showed promising results in treating patients during the Middle East Respiratory Syndrome (MERS) outbreaks, was approved for emergency use against SARS-CoV-2 in January 2020. Remdisivir blocks ribonucleic acid (RNA)-dependant-RNA polymerase (RdRP) by acting as a chain terminator, thus preventing the production of new viral RNA and viral replication. Hydroxychloroquine was assumed to operate by the same principle; however, further evidence showed worrying side effects.
Acetaminophen and paracetamol both work through the other mechanism. The high fever triggered by SARS-CoV-2 infection is caused by the elevation of pyrogenic cytokines like interleukins, which signal receptors such as prostaglandin E2 (PCE2). Acetaminophen reduces the production of PGE2, which subsequently reduces the fever, thus resulting in less death among the endothelial cells surrounding the lungs. Other drugs, such as tocilizumab and Anankira, block interleukin receptors in an attempt to accomplish the same outcome.
Researchers from University Malaysia Terengganu have been investigating the ability of some microalgae metabolites to prevent cytokine storm syndrome during coronavirus disease 2019 (COVID-19). To this end, the researchers focus on molecules that could imitate the effects of these drugs, with the aim of using these alongside existing generic drugs. Cytokine storm normally arises due to the most severe inflammatory responses to viral infection and can be caused by the overactivation of many different signaling pathways.
The renin-angiotensin system (RAS) is used to maintain the homeostasis of vascular functions in Isochrysis zhanjiangenesis. As part of this system, a novel peptide has shown the ability to block angiotensin-converting enzyme (ACE).
The receptor-binding domain (RBD) on the S1 subunit of the spike protein of SARS-CoV-2 binds to the ACE-2 receptor on the host cell in order to permit viral cell entry. However, the compromise of ACE-2 can also lead to higher levels of angiotensin II (Ang-II) in the blood, thus resulting in aberrant RAS signaling, amplified cytokines in the bloodstream, and, as a result, increased inflammation.
ACE converts Ang-I into the active form, Ang-II. This unique peptide could help reduce inflammation by lowering the level of Ang-II in the blood by blocking ACE. Application of the peptide on cells in culture showed reduced levels of adhesion molecules and a pathway by which oxidative stress could be reduced.
Study findings
The nuclear factor kappa-light-chain-enhancer of activated B-cells (NF-kB) and mitogen-cctivated protein kinase (MAPK) pathways both play key roles in inflammation. More specifically, the NF-kB pathway stimulates the Janus kinase/signal transducer and activates of transcription (JAK/STAT3) pathway, which results in the transcription of multiple immune-modulating and immune-stimulating genes. NF-kB also governs many other inflammatory responses.
The researchers identified several microalgae extracts that act on the NF-kB pathway by down-regulating related cytokines including carotenoids, whole-cell extracts, and certain peptides. Previous research as revealed that when SARS-CoV-2 infection leads to the activation of IkB kinase (IKK) through pattern recognition receptors (PRR), pathogen-associated molecular patterns (PAMPs), and myeloid differentiation factor 88 (MyD88), the activated IKK then catalyzes the phosphorylation of IkB, releasing NF-kB. This can then activate NF-kB target genes, activating more pro-inflammatory cytokines and other molecules that lead to extensive inflammation.
The aforementioned peptides and carotenoids, as well as a molecule called violaxanthin, have shown the ability to reduce translocation of NF-kB p65/50 dimers into the nucleus, thus preventing the following cascade of inflammatory signals.
Cyclooxygenase 2 (Cox-2) is an enzyme known to inhibit products of the arachidonic acid (AA) pathway, which produces eicosanoids that act as regulators of the NF-kB pathways. These eicosanoids are also involved in the cyclooxygenase (COX) and lipooxygenase (LO) pathways. Metabolites from several microalgae have been identified that show the same ability as Cox-2, of which includes oxylipins, peptides, sterols, carotenoids, and lipids.
Only two clinical trials have examined the ability of microalgae metabolites in humans. While neither of these trials focused on COVID-19, the diseases they have examined have known inflammation pathologies including the activation of many of the aforementioned pathways.
One study focuses on rheumatoid arthritis, with patients given a supplement from Schizochytrium sp. that competes with arachidonic acid (AA) during eicosanoid production, thus reducing blood serum levels of pro-inflammatory products from the AA pathway. The other study supplied Chlorella vulgaris tablets to patients with non-alcoholic fatty liver disease, which showed strong anti-inflammatory products.
The success of these trials suggests that microalgae metabolites are safe for use in humans. While drugs from microalgae metabolites are likely a long way from development, they could provide a powerful tool against future pandemics with inflammation pathologies.
Journal reference:
- Wan Afifudeen, C. L., Teh, K. Y. & Cha, T.S. (2021). Bioprospecting of microalgae metabolites against cytokine storm syndrome during COVID-19. Molecular Biology Reports. doi:10.1007/s11033-021-06903-y