The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first detected through the coronavirus disease 2019 (COVID-19) that it caused, in Wuhan, China, at the end of 2019.
Many attempts are being made to develop a drug that will inhibit the replication of this virus, especially in the face of newly emerging variants of the pathogen that threaten to be more pathogenic and highly transmissible, compared to the wild-type.
A new study, available on the bioRxiv* preprint server while the article undergoes peer review, describes the antiviral activity of a compound called atazanavir (ATV) that specifically inhibits the main protease enzyme of SARS-CoV-2. This could help develop better antivirals than remdesivir, which is all that is currently available among this category of drugs.
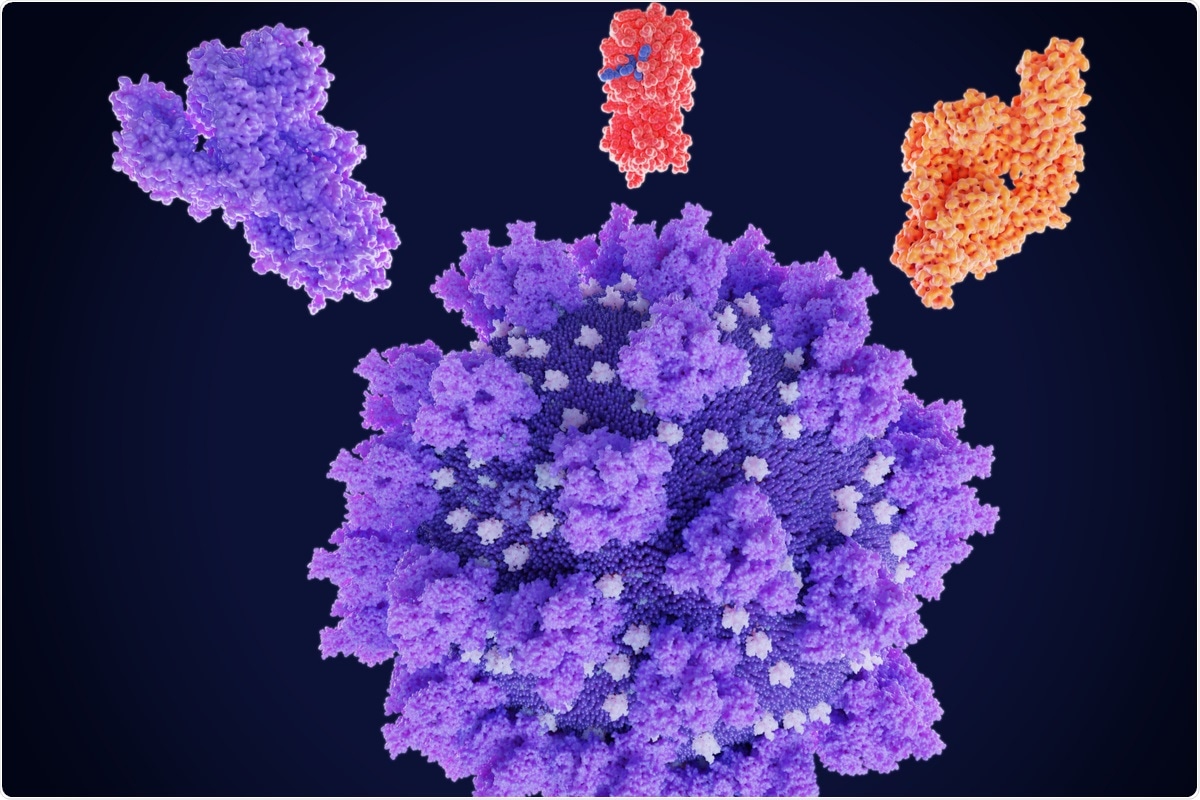 Study: Atazanavir is a competitive inhibitor of SARS-CoV-2 Mpro, impairing variants replication in vitro and in vivo. Image Credit: Juan Gaertner/Shutterstock
Study: Atazanavir is a competitive inhibitor of SARS-CoV-2 Mpro, impairing variants replication in vitro and in vivo. Image Credit: Juan Gaertner/Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
ATV is a drug used to treat human immunodeficiency virus (HIV) infection, a protease inhibitor. The current authors showed in their earlier work that it has activity against SARS-CoV-2, both by modeling and in cell-based assays.
Though it was explored as a potentially useful drug against COVID-19 through clinical trials, this was unproductive because the necessary preclinical testing had not been carried out. There was no consensus on how it acts, or how effective it is against the virus. It is one of many repurposing efforts that have not yielded any discernible benefit in the fight against the virus.
It has become clear that in order to cut down on the wastage of such efforts, these drugs must first be studied for their mechanism of action, in vitro and in vivo activity against viral biological processes, and their interactions with the viral enzyme target as well as with the type II pneumocytes.
Recent studies based on bioinformatics and pharmacological research, including enzyme inhibition curves, shows that ATV does, indeed, act on the SARS-CoV-2 Mpro enzyme. This key enzyme cleaves 11 sites on the large viral polyprotein, and thus produces the essential proteins for viral replication.
The viral Mpro is the target of the drug PAXLOVID™ developed by Pfizer, which has been shown to prevent 80% of hospitalizations, indicating the need to characterize the pharmacologic features of drugs that act on this enzyme. This would help understand the optimal drug targets in order to develop next-generation antivirals.
What did the study show?
The current study looks at how ATV acts on the Mpro enzyme. The scientists compared the inhibition produced by ATV with that of boceprevir, or GC376, finding that the inhibition was somewhat less with the latter, at ~200 vs ~700 nM, respectively.
The drug produced competitive inhibition specifically of the drug, but not of the viral papain-like protease (PLpro). This requires the presence of catalytic water (H2Ocat), at the catalytic site of the Mpro enzyme. They found that apart from wildtype SARS-CoV-2, the drug is also active against the B.1 and Gamma strains of the virus, inhibiting their entry into the Calu-3 cell line derived from pneumocytes type II.
The Gamma strain was more susceptible than the earlier B.1 lineage from which it was derived, to both ATV and remdesivir. For both drugs, the therapeutic margin was wide enough to suggest clinical potential.
In mice models, the drug was found to reach therapeutic concentrations within the plasma and to concentrate in the lungs. Moreover, it improved the survival of infected mice expressing the human angiotensin-converting enzyme 2 (hACE2), when they were treated 12 hours post-infection with ATV. In untreated animals, the mortality is 100% within six days; this was reduced in the treated group.
Finally, it also reduced the inflammation induced by the virus, and prevented cell death, as seen by the examination of bronchoalveolar lavage (BAL). It also mitigated lung damage in infected animals on treatment with the drug. This is due to its anti-inflammatory and antiviral activity, as shown earlier by its ability to reduce the level of SARS-CoV-2-induced cytokine secretion in the monocytes, and pyroptosis due to viral infection.
What are the implications?
Repurposing of clinically approved drugs was thought to be a good way to speed up the development of antivirals against SARS-CoV-2. However, the poor success of this strategy, compared to the better performance of oral antiviral drugs like PAXLOVID™ or molnupiravir, that do reduce hospitalization rates, indicate the central role of detailed preclinical evaluation of a drug.
Earlier, ATV’s anti-SARS-CoV-2 activity was missed in some repurposing studies, because of the need for catalytic water, which is required at the His-41 residue of Mpro, to catalyze proteolytic cleavage.
The current study went through the classical steps of cell-based assays and animal models to pave the way for further clinical development of the drug, utilizing the knowledge of the target concentration in plasma and the need for catalytic water. This could lead to analogs that act differently from PAXLOVID™, which binds covalently to the catalytic cysteine to inhibit the enzyme.
The results show that ATV has a different antiviral activity against the virus compared to PAXLOVID™, which encourages further research on drugs acting at the Mpro-ATV interface. Further studies are required to find the dosage at which this drug shows clinical activity against SARS-CoV-2. Compared to the extant literature, ATV can be tolerated short-term at dosages threefold those used in lifelong HIV treatment.
Our studies may contribute to a better comprehension of the Mpro/ATV interaction, which could pave the way to the development of specific inhibitors of this viral protease.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Chaves, O. A. et al. (2021). Atazanavir Is a Competitive Inhibitor Of SARS-Cov-2 Mpro, Impairing Variants Replication In Vitro And In Vivo. bioRxiv preprint. doi: https://doi.org/10.1101/2021.11.24.469775. https://www.biorxiv.org/content/10.1101/2021.11.24.469775v1
- Peer reviewed and published scientific report.
Chaves, Otávio Augusto, Carolina Q. Sacramento, André C. Ferreira, Mayara Mattos, Natalia Fintelman-Rodrigues, Jairo R. Temerozo, Leonardo Vazquez, et al. 2022. “Atazanavir Is a Competitive Inhibitor of SARS-CoV-2 Mpro, Impairing Variants Replication in Vitro and in Vivo.” Pharmaceuticals 15 (1): 21. https://doi.org/10.3390/ph15010021. https://www.mdpi.com/1424-8247/15/1/21.