The coronavirus disease 2019 (COVID-19) has been caused by the rapid outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus and has already claimed more than 5.28 million lives worldwide. Long COVID or post-acute sequelae of SARS-CoV-2 (PASC) affect between 10-30% of patients and is a long-term manifestation of acute COVID-19.
Scientists have defined PASC as the emergence or persistence of symptoms extending beyond four weeks from the start of acute illness. Many reports of cardiopulmonary symptoms associated with PASC have been documented. However, research on cardiovascular manifestations remains limited.
In a new study published on the medRxiv* preprint server, scientists discuss the characteristics, diagnostic evaluations, and cardiac diagnoses in patients who were referred to a cardiovascular disease clinic designed for patients with PASC.
 Study: Characteristics of Patients Referred to a Cardiovascular Disease Clinic for Post-Acute Sequelae of SARS-CoV-2 Infection. Image Credit: Alessandro Pintus / Shutterstock.com
Study: Characteristics of Patients Referred to a Cardiovascular Disease Clinic for Post-Acute Sequelae of SARS-CoV-2 Infection. Image Credit: Alessandro Pintus / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
About the study
This was an observational study, where the sample included all individuals who were referred to the Yale cardiovascular clinic for PASC between May 2020 and September 2021. Diagnostic evaluation of the patients included vital signs, cardiopulmonary physical examination, electrocardiogram (ECG), laboratory studies, and echocardiogram.
Scientists were able to manually extract this information from the electronic medical record. N-terminal (NT) pro-hormone BNP (NT-proBNP_, troponin, d-dimer, and C-reactive protein (CRP) tests were only conducted based on clinical suspicion.
In patients with orthostatic intolerance, a stand test for postural orthostatic tachycardia syndrome (POTS) was conducted. Further investigation was carried out to detect cardiovascular disease pathology and understand cardiovascular symptoms that were not readily attributable to a cardiovascular diagnosis.
In the current study, the researchers describe the clinical characteristics and diagnostic yield of testing. They also reported the predictors of having cardiovascular symptoms without an identified diagnosis.
Study findings
Of the 126 patients included in the study, the average age was 44 years, 9% were above 65 years of age, and 66% were female. About 24% of the patients were hospitalized due to acute COVID-19, of which 9% and 11% of patients were critically and severely ill, respectively.
A total of 120 patients had confirmed antigen studies for COVID-19. Primary care (54%), pulmonology (26%), and cardiology (12%) were the top three sources of referrals.
The patients also had comorbidities such as hypertension (23%), hyperlipidemia (25%), diabetes (17%), and obesity (37%), whereas 10% of patients had underlying cardiovascular disease and 32% had an underlying pulmonary or rheumatologic disease. The most common cardiovascular symptoms included dyspnea (52%), chest pain/pressure (48%), and palpitations (44%), with 84% of patients exhibiting at least one of these symptoms.
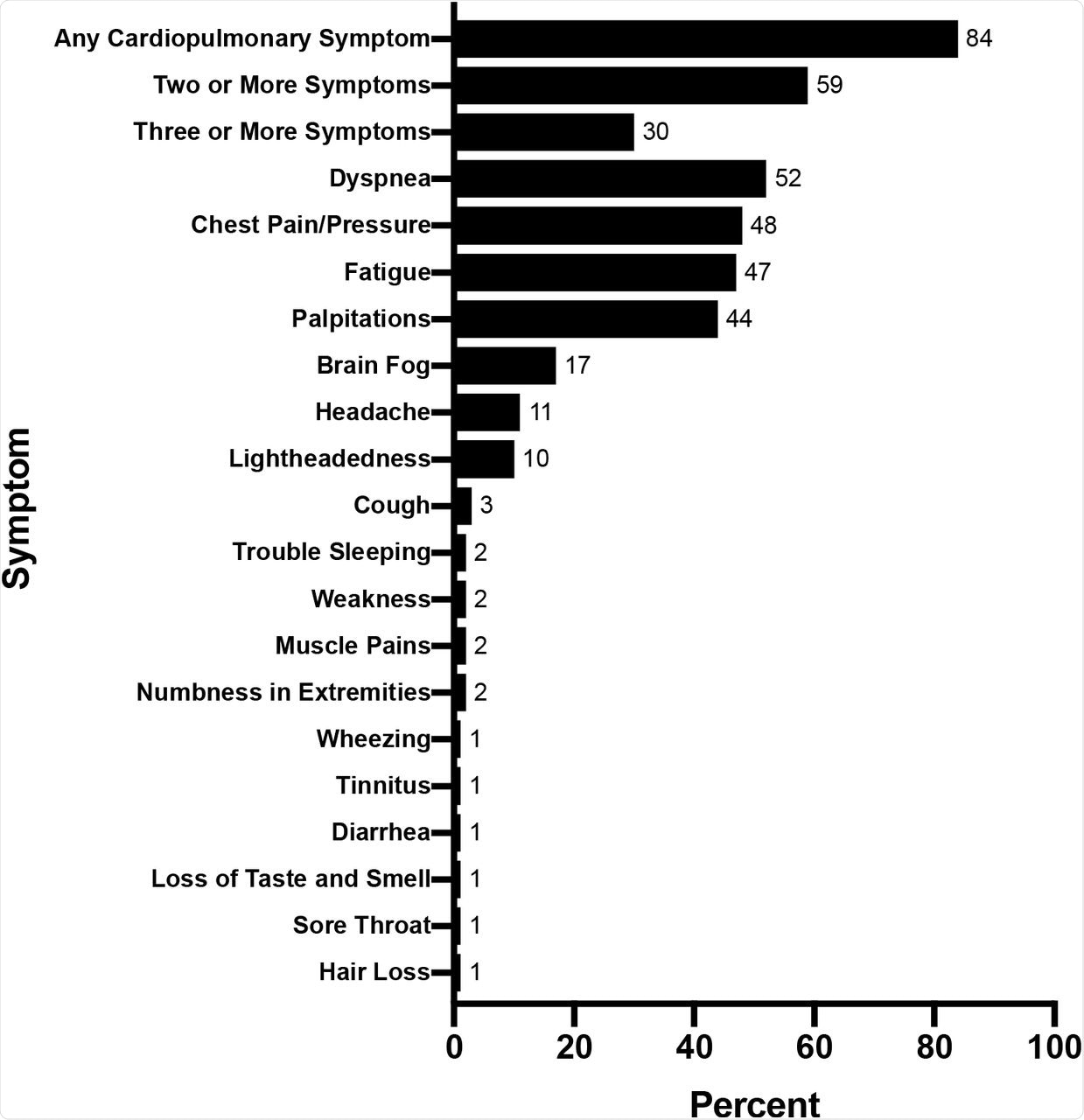 Baseline Symptoms of Patients Referred for Cardiovascular Symptoms associated with Post-Acute Sequelae of SARS-CoV-2 (PASC).
Baseline Symptoms of Patients Referred for Cardiovascular Symptoms associated with Post-Acute Sequelae of SARS-CoV-2 (PASC).
The current study shows that cardiovascular manifestations of PASC are common and mainly affect non-elderly individuals. Only 23% of patients suspected to have a cardiac etiology led to a cardiovascular diagnosis, including new cardiomyopathy, ischemia, arrhythmias, and myocardial involvement.
Many patients suffered from exercise intolerance, describing fatigue on performing activities of daily living. However, in the majority of cases (77%), cardiovascular disease was not detected.
While many individuals also suffered from “brain fog,” characterized by memory problems, difficulty concentrating, and sleep disturbance, others also reported body aches. It is important to note that these symptoms overlap with myalgic encephalomyelitis-chronic fatigue syndrome (ME-CFS).
Previous research has shown that COVID-19 could impact the cardiovascular system through several mechanisms. These mechanisms could include viral injury, inflammation, dysregulation of the angiotensin-converting enzyme 2 (ACE-2), along with metabolic and autonomic impairment. However, these are difficult to discern in a standard clinical evaluation.
In some patients who underwent invasive coronary vasomotion testing and cardiopulmonary exercise testing, scientists observed downstream physiological dysregulation. Calcium channel blockers, nitrates, statins, and L-arginine were prescribed for these patients.
The majority of patients had low peak maximal oxygen consumption (VO2) with normal cardiac and pulmonary function. This could have been secondary to bedrest deconditioning and/or impaired oxygen extraction. For all patients with exercise intolerance, scientists employed principles from the Levine protocol, which was developed for patients with POTS.
Limitations
It must be noted that the referrals and diagnostic evaluations were not systematic and they could be generalized to other practices witnessing high volumes of patients with PASC. Further, scientists point out that the understanding of PASC evolved with time, which led to the reduction in the number of diagnostic tests.
Despite these limitations, all patients had a thorough cardiovascular physical exam, ECG, and echocardiogram. New diagnoses that better define the PASC cardiovascular syndrome may emerge; however, the diagnostic algorithms need to be further developed.
Conclusion
The current study provides new insights into patients with cardiovascular manifestations of PASC. The findings discussed here emphasize the need for rapid research and multidisciplinary teams to treat a heterogenous group of COVID-19 patients.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Wang, Y. S., Adejumo, P., See, C., et al. (2021) Characteristics of Patients Referred to a Cardiovascular Disease Clinic for Post-Acute Sequelae of SARS-CoV-2 Infection. medRxiv. doi:10.1101/2021.12.04.21267294. https://www.medrxiv.org/content/10.1101/2021.12.04.21267294v1.
- Peer reviewed and published scientific report.
Wang, Stephen Y., Philip Adejumo, Claudia See, Oyere K. Onuma, Edward J. Miller, and Erica S. Spatz. 2022. “Characteristics of Patients Referred to a Cardiovascular Disease Clinic for Post-Acute Sequelae of SARS-CoV-2 Infection.” American Heart Journal Plus: Cardiology Research and Practice 18 (June): 100176. https://doi.org/10.1016/j.ahjo.2022.100176. https://www.sciencedirect.com/science/article/pii/S2666602222000933.