A team of US-based scientists has recently explored various risk factors associated with the poor prognosis of coronavirus disease 2019 (COVID-19). They have identified thrombosis-related risk factors as a major predictor of in-hospital COVID-19 related mortality. The study is currently available on the medRxiv* preprint server while awaiting peer review.
 Study: Time-Varying Mortality Risk Suggests Increased Impact of Thrombosis in Hospitalized Covid-19 Patients. Image Credit: NIAID
Study: Time-Varying Mortality Risk Suggests Increased Impact of Thrombosis in Hospitalized Covid-19 Patients. Image Credit: NIAID

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen of the COVID-19 pandemic, is a deadly RNA virus belonging to the human beta-coronavirus family. Being a respiratory virus, it primarily affects the upper and lower respiratory tracts and causes severe lung pathologies in susceptible individuals. However, in critically ill COVID-19 patients, SARS-CoV-2 infection has been found to associate with hyperinflammation and thrombosis.
The changing characteristics of COVID-19 disease according to pre-existing health conditions of patients has made it necessary to identify the major predictive biomarkers of disease severity and mortality.
In the current study, the scientists have investigated inflammation, thrombosis, and other risk factors on in-hospital COVID-19 related mortality.
Study design
The study was conducted on more than 4,000 COVID-19 patients who had been hospitalized between March 2020 and August 2021. All tested biomarkers were broadly categorized into three main groups, including thrombosis, inflammation, and other risk factors (demographics, vital signs, comorbidities, and lab tests on admission). For thrombosis risk, high D-dimer and high hematocrit were considered. High C-reactive protein (CRP), high Neutrophil/Lymphocyte ratio, and low serum albumin were considered for inflammation risk.
A generalized additive model was used to investigate the changing impact of tested biomarkers on in-hospital mortality over time. Specifically, the impact of each biomarker on mortality risk was estimated for each day. In addition, the mean mortality risk associated with thrombosis biomarkers and inflammation biomarkers was estimated after adjusting the contributions of all other risk factors.
Important observations
A gradual increase in mortality risk from thrombosis-related biomarkers was observed over time in hospitalized COVID-19 patients. The increase in thrombosis-related risk was associated with a decrease in inflammation-related risk over time. The mortality risk from other tested biomarkers mostly remained unchanged during the study period except for the high ferritin level, which showed a gradually increased association with mortality risk over time.
In March 2010, the overall mortality risk was 20%, which gradually reduced to 3% in August 2021. A similar reduction in mortality risk was observed in patients with at least one inflammation-related biomarker. In contrast, the mortality risk of patients with at least one thrombosis-related biomarker reduced from 22% in March to 6% in August.
Notably, an association between change in mortality risk and change in treatment type was observed during the study period. In addition, a trend towards increased usage of glucocorticoids and anti-coagulants was observed for most of the patients.
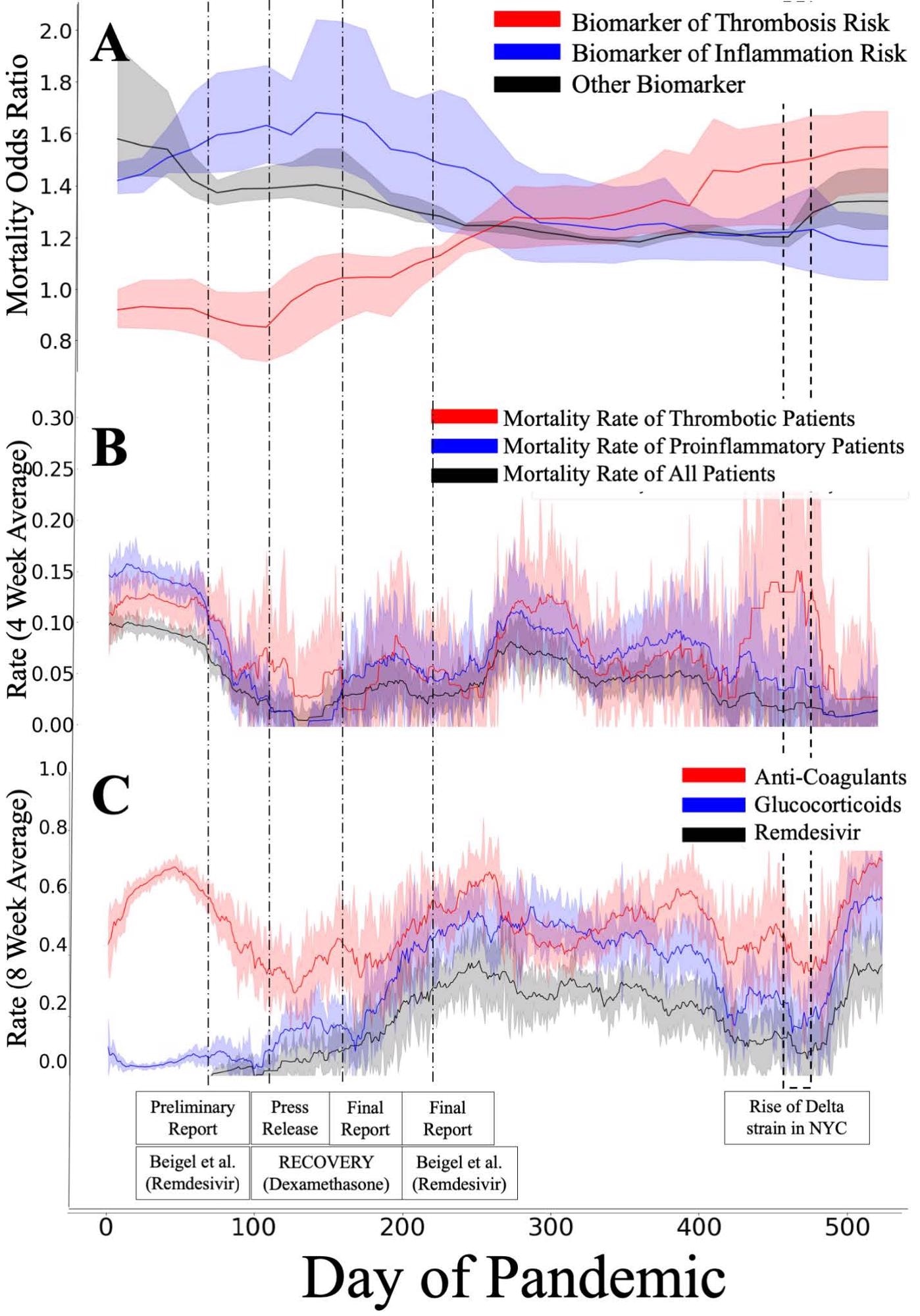 (A) The predictive power of biomarkers has changed over time. Biomarkers of inflammation risk (elevated C-reactive protein, low albumin, high Neutrophil/Lymphocyte ratio) were initially powerful predictors of in-hospital mortality, but have become less predictive over time. In contrast, biomarkers of thrombosis risk (elevated D-Dimer, elevated hematocrit) are more predictive of mortality in August 2021 than during March 2020. This suggests that the successful treatment of patients hospitalized with indicators of thrombosis risk has lagged behind the treatment of other groups. (B) The in-hospital mortality rate has decreased over time for all patients, but at a reduced rate for patients satisfying at least one biomarker rule for thrombosis risk. (C) Treatment protocols have changed over time, with a trend toward glucocorticoid and anticoagulant prescription (overwhelmingly prophylactic heparin) for the majority of patients. We mark the dates of several important publications and the rise of the Delta strain in NYC.
(A) The predictive power of biomarkers has changed over time. Biomarkers of inflammation risk (elevated C-reactive protein, low albumin, high Neutrophil/Lymphocyte ratio) were initially powerful predictors of in-hospital mortality, but have become less predictive over time. In contrast, biomarkers of thrombosis risk (elevated D-Dimer, elevated hematocrit) are more predictive of mortality in August 2021 than during March 2020. This suggests that the successful treatment of patients hospitalized with indicators of thrombosis risk has lagged behind the treatment of other groups. (B) The in-hospital mortality rate has decreased over time for all patients, but at a reduced rate for patients satisfying at least one biomarker rule for thrombosis risk. (C) Treatment protocols have changed over time, with a trend toward glucocorticoid and anticoagulant prescription (overwhelmingly prophylactic heparin) for the majority of patients. We mark the dates of several important publications and the rise of the Delta strain in NYC.
Study significance
The study identifies thrombosis-related biomarkers as potent predictors of in-hospital COVID-19 related deaths. Although a general trend towards steroid-based and anti-coagulant-based treatments has been observed during the study period, the risk of mortality in patients with thrombosis remains higher than that in patients with inflammation.
As mentioned by the scientists, negative consequences of thrombosis observed in the study could be due to the unavailability of appropriate anti-coagulants and thrombolytic drugs. Although heparin is commonly used as an anti-coagulant, its efficacy in preventing thrombosis in COVID-19 patients is still uncertain. One possible reason is the reliance of heparin on endogenous antithrombin, which is known to reduce during SARS-CoV-2 infection. Therefore, the scientists suggest that anti-coagulants that do not reply on antithrombins, such as Argatroban or Bivalirudin, could be more beneficial than heparin in preventing thrombosis in COVID-19 patients.
Overall, the study highlights the need for more research on COVID-19 patients who have thrombosis or are at higher risk of developing thrombosis in order to improve disease prognosis and reduce mortality.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.