The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was first discovered in patients with severe pneumonia at the end of 2019, has since infected over 272 million worldwide and caused the deaths of over 5.3 million people.

Study: An Update on the Relationship of SARS-CoV-2 and Male Reproduction. Image Credit: Anna Tryhub / Shutterstock.com
In a recent Frontiers in Endocrinology study, researchers provide a review on the molecular mechanism of viral tropism, post-infection clinical characteristics, and potentially harmful consequences on the male reproductive system in COVID-19 patients. Moreover, the findings from the current study provide acceptable conclusions about the impact of COVID-19 on male reproduction and propose new research directions.
Can SARS-CoV-2 be detected in semen?
SARS-CoV-2 is primarily transmitted through the air by droplets containing virions according to research published in early 2020. These infected droplets then enter the nose and mouth, where they can ultimately reach and infect the upper respiratory tract.
The recognition of the ACE2 receptor is required for SARS-CoV-2 entrance into host cells. Because the viral spike (S) protein binds to the extracellular domain of the ACE2 receptor, the transmembrane protease serine protease-2 (TMPRSS2) is needed for S protein cleavage at the S1/S2 location, which subsequently leads to viral membrane fusion.
After SARS-CoV-2 reaches host cells, the viral ribonucleic acid (RNA) genome begins to multiply and instruct host cell ribosomes to translate structural proteins and polyproteins for the viral capsid. In order to disseminate the infection, viral particles are formed in the reticulum-Golgi intermediate compartment (ERGIC) and then released by exocytosis.
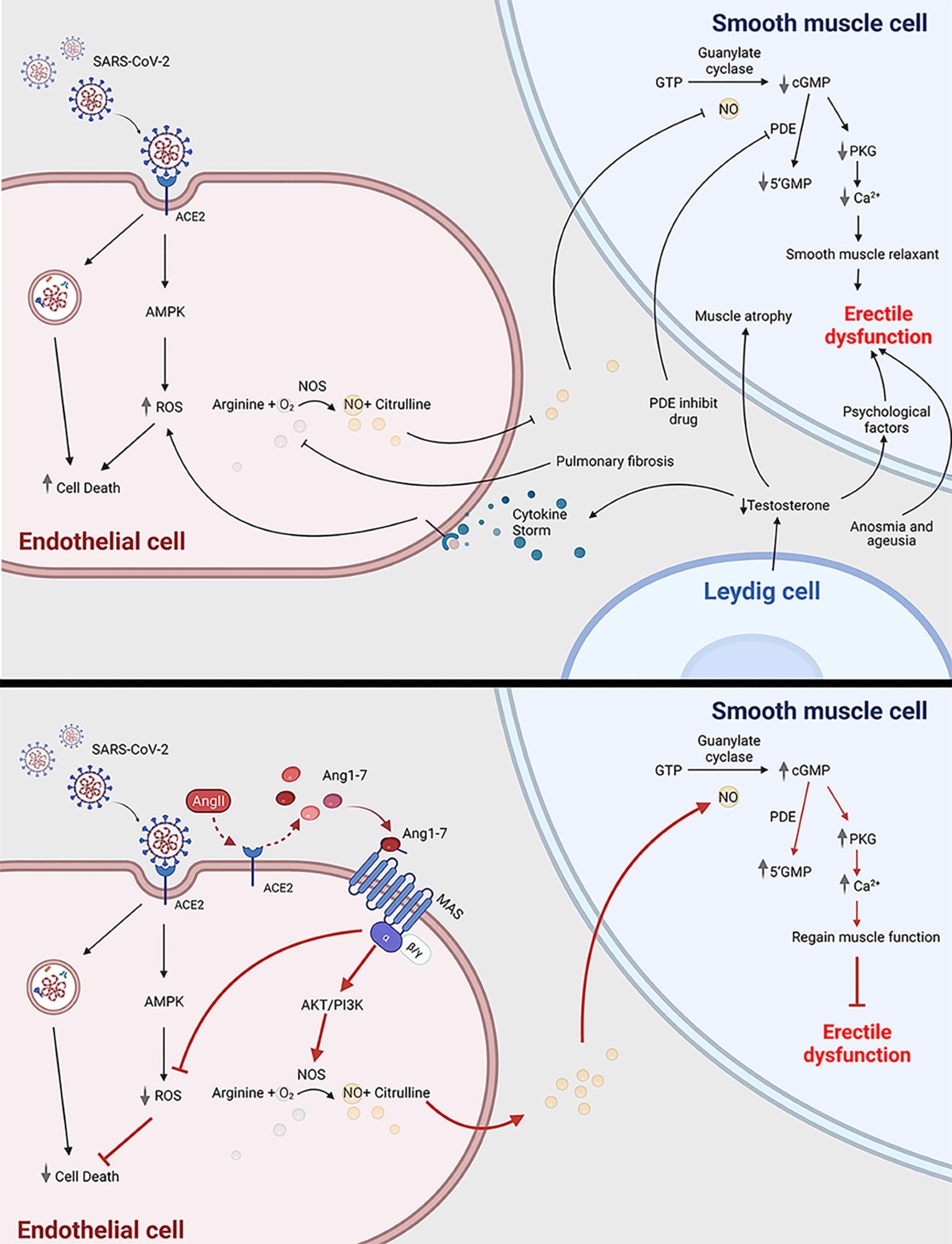 COVID-19 can cause erectile dysfunction. The potential mechanism of how COVID-19 infection is related to erectile dysfunction through impairing endothelial cell and smooth muscle cell (top panel); Ang1-7 is a potential novel drug target to treat erectile dysfunction in COVID-19 patients (bottom panel). ACE2, angiotensin-converting enzyme 2; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ED, erectile dysfunction; ROS, reactive oxygen species; AMPK, AMP-activated protein kinase; Ang1-7, angiotensin 1-7; Ang II, angiotensin 2; PDE, phosphodiesterase; 5’GMP, Guanosine-5’-monophosphate; cGMP, cyclic guanosine monophosphate; PKG, Cyclic GMP–dependent protein kinase; NOS, nitric oxide synthase. This scheme was created using BioRender, accessed on Sept. 29, 2021.
COVID-19 can cause erectile dysfunction. The potential mechanism of how COVID-19 infection is related to erectile dysfunction through impairing endothelial cell and smooth muscle cell (top panel); Ang1-7 is a potential novel drug target to treat erectile dysfunction in COVID-19 patients (bottom panel). ACE2, angiotensin-converting enzyme 2; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ED, erectile dysfunction; ROS, reactive oxygen species; AMPK, AMP-activated protein kinase; Ang1-7, angiotensin 1-7; Ang II, angiotensin 2; PDE, phosphodiesterase; 5’GMP, Guanosine-5’-monophosphate; cGMP, cyclic guanosine monophosphate; PKG, Cyclic GMP–dependent protein kinase; NOS, nitric oxide synthase. This scheme was created using BioRender, accessed on Sept. 29, 2021.
Several viruses, including Zika and the human immunodeficiency virus (HIV), have been known to penetrate the blood-testis barrier (BTB) and transfer sexually. The presence of SARS-CoV-2 in sperm is currently debatable.
A semen test of 38 specimens revealed that 6 samples were positive for SARS-CoV-2, including 4 of 15 patients in the acute stage of infection and 2 of 23 individuals recovering from COVID-19. During the acute stage, patients may have a high blood viral load, which permits the virus to have a better chance of reaching the testes and entering the BTB through local and/or systemic inflammation. In most studies, there was no evidence of viral infection in the sperm.
Recently, there has been some skepticism about favorable outcomes, as ejaculation and semen collection processes may be polluted. To understand the situation, more data must be collected in accordance with World Health Organization (WHO) guidelines to avoid virus infection. However, the sensitivity and specificity of the reverse-transcription-polymerase chain reaction (RT-PCR) methods used to detect SARS-CoV-2 in seminal fluid have not been assessed in almost all instances.
It remains unclear whether existing detection methods for nasopharyngeal swabs are suitable for virus detection in sperm. Although most studies show a low risk of seminal infection, infection in sperm and gametes remains a concern.
Thus, more epidemiological data on viral transmission from male recovered patients to previously unaffected sexual partners is needed. It is also critical to identify SARS-CoV-2 in cryopreserved semen samples, as the virus can maintain its biological pathogenicity in liquid nitrogen.
COVID-19 and erectile dysfunction
Concerns regarding the potential for COVID-19 survivors to develop erectile dysfunction (ED) (ED) as a result of the infection's high transmissibility and greater severity rates in males than in women have also been raised. After addressing the probable bias coming from age and body mass index (BMI), characteristics that contribute to both higher prevalence of ED, a preliminary investigation showed that ED and COVID-19 appear to be substantially linked.
In previous studies, most male COVID-19 participants had lower testosterone levels, thus indicating hypogonadism. Hypogonadism in COVID-19 patients may be caused by testis injury, including decreased Leydig cells and poor steroidogenesis.
Low testosterone promotes vascular smooth muscle cell atrophy by suppressing the production of nitric oxide synthase. Furthermore, testosterone suppresses the immune system. Low testosterone in COVID-19 patients can indicate poor prognosis and mortality.
Implications
COVID-19 appears to have an impact on various areas of male reproduction, including the reproductive tracts, hormones, gametes, and sexual function. COVID-19 has the potential to cause orchitis or epididymitis, compromising testicular integrity and spermatogenesis.
Patients with COVID-19 have lower sperm concentration and motility. However, there appears to be some disagreement regarding the presence of SARS-COV-2 in the sperm and testis. Furthermore, because COVID-19 patients have a significant risk of ED, the authors proposed angiotensin as a novel therapeutic target for ED in COVID-19.
The current review also examines the toxicity of medications targeting COVID-19 on the reproductive tract, as well as recent research in adjacent disciplines and how developing models might be used to assist in such studies. Taken together, there are still unanswered questions regarding the impact of COVID-19 on the male reproductive system.
Journal reference:
- Guo, J., Sheng, K., Wu, S., et al. (2021). An Update on the Relationship of SARS-CoV-2 and Male Reproduction. Frontiers in Endocrinology. doi:10.3389/fendo.2021.788321