A massive effort has been made to find preventive measures and effective coronavirus disease 2019 (COVID-19) treatments. Unfortunately, there have been approximately 306 million confirmed cases, and more than 5.48 million people have died from the disease. It has been proposed that influenza vaccination may provide some protection against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), resulting in its recommendation as a preventive measure against COVID-19. Host-immune responses to both viruses supported this theory. However, there have been concerns about the interaction between influenza vaccination and the risk of SARS-CoV-2 infection.
The study
A new study published in The Journal of Infectious Diseases examined if influenza vaccination altered the risk of SARS-CoV-2 infection and clinical outcomes of COVID-19. The study included health care workers (HCWs) from Denmark who were offered influenza vaccination.
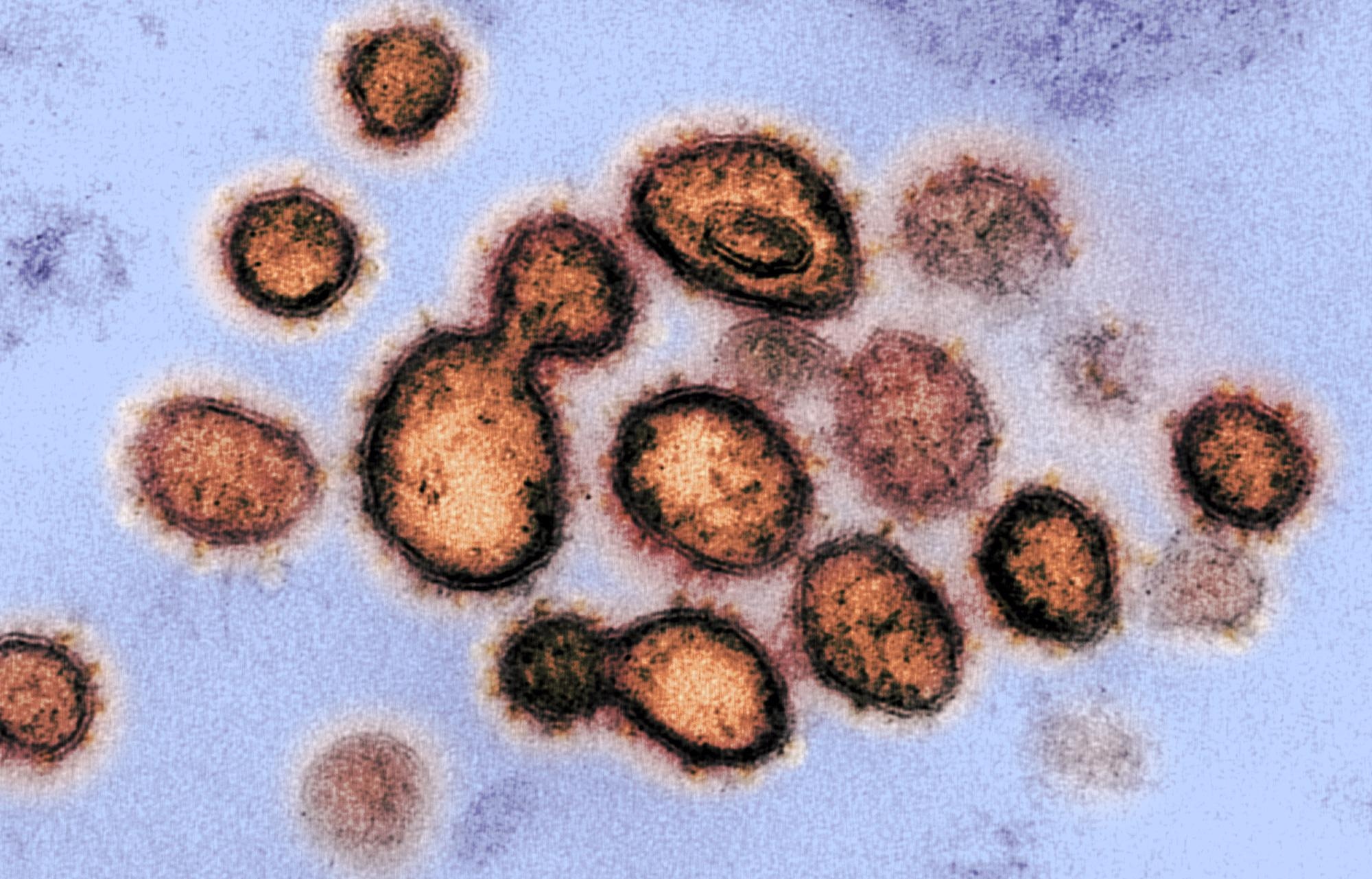 Study: Effect of influenza vaccination on risk of COVID-19 – A prospective cohort study of 46,000 health care workers. Image Credit: NIAID
Study: Effect of influenza vaccination on risk of COVID-19 – A prospective cohort study of 46,000 health care workers. Image Credit: NIAID
This prospective cohort study conducted repeated measurements of antibodies against SARS-CoV-2 among HCWs at hospitals, specialized health care institutions, and in the primary sector in the Capital Region and the Region of Zealand in Denmark—estimating a total of 60,681 HCWs. Antibody screening was carried out three times during 2020; participants in the second and third screening rounds were not required to have participated previously.
Overall, 48,709 HCWs completed the questionnaire; information on influenza vaccination was available for 46,112 participants. In addition, information on influenza vaccination and antibody status against SARS-CoV-2 was available for 34,366 and 35,168 participants between 2018-2019 and 2019-2020, respectively. Among these 3,379 participants had either symptomatic infections or hospitalization.
Findings
The results revealed that the influenza-vaccinated participants were older, more educated, and had more comorbidities than the unvaccinated participants. The risk ratios (RRs) of symptomatic COVID-19 were 1.03 and 1.02 for vaccinated compared with unvaccinated HCWs for the seasonal vaccination in 2019-2020 and 2018-2019, respectively. Whereas, the RRs of developing antibodies to SARS-CoV-2 in participants vaccinated against influenza virus were 1.01 and 0.93 compared with unvaccinated participants for the seasonal vaccination during the same periods.
Additionally, adjusted odds ratios (ORs) for hospitalization of 0.91 and 0.89 were found when comparing influenza vaccinated with unvaccinated participants during 2019-2020 and 2018-2019, respectively. While the corresponding adjusted ORs for symptomatic COVID-19 were 1.24 and 1.16, respectively, and adjusted ORs for developing antibodies against SARS-CoV-2 were 1.06 and 1.00, respectively.
In a subgroup analysis of 1,841 participants aged ≥65 years, the RRs of developing antibodies against SARS-CoV-2 were 0.93 and 0.99 for influenza vaccinated individuals compared to the unvaccinated participants during 2019-2022 and 2018-2019, respectively. There was no significant effect of influenza vaccination for 88 participants aged ≥65 years on hospitalization or being symptomatic for either season.
Discussion
Hence, the findings showed that vaccination against influenza did not change the risk of hospitalization or symptoms due to COVID-19, nor did influenza vaccination alter the risk of contracting SARS-CoV-2 infection.
The current study coincides with the previous null-effect studies on infection with SARS-CoV-2 as measured by pharyngeal swabs or serology. A comparison of vaccinated to unvaccinated individuals has been presented for the first time in this study.
A significant limitation of this study is that the information on the severity of COVID-19 is based on a questionnaire filled in by participants; contemporary hospitalizations may be underreported.
From the results of this study, it was inferred that influenza vaccination does not affect the risk of SARS-CoV-2 infection or COVID-19 disease.
Journal reference:
- Kristensen, J., Hasselbalch, R., Pries-Heje, M., Nielsen, P., Dehlbæk Knudsen, A., & Fogh, K. et al. (2022). Effect of influenza vaccination on risk of COVID-19 – A prospective cohort study of 46,000 health care workers. The Journal Of Infectious Diseases. https://doi.org/10.1093/infdis/jiac001, https://academic.oup.com/jid/advance-article/doi/10.1093/infdis/jiac001/6497955