The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) delta variant, dominant in most communities, was primarily fueling the summer surge of coronavirus disease 2019 (COVID-19) in the United States in 2021.
The SARS-CoV-2 delta variant has increased transmissibility, resulting in increased cases and a commensurate increase in hospitalization rates in many locales, particularly in areas where COVID-19 immunization rates are low. As a result, vaccination and other public health mitigation methods like masking and social separation are being used to try to stop the outbreak.
The US Food and Drug Administration (FDA) has approved anti-spike monoclonal antibodies for the early treatment of mild to moderate COVID-19 in high-risk patients. As a result, Mayo Clinic launched the Monoclonal Antibody Treatment Program (MATRx) in November 2020 to give these treatments to high-risk patients outside of the hospital setting.
More than 13,800 patients had received anti-spike monoclonal antibodies by October 22, 2021, according to the program. In comparison to a propensity score-matched sample of 2,335 untreated individuals, the program's outcomes demonstrated a substantial reduction in hospital and critical care unit admission and mortality in 2,335 patients who received bamlanivimab infusion.
In this research paper, a group of Mayo Clinic researchers discusses how data from MATRx's clinical prioritizing algorithms can be used to address anti-spike monoclonal antibody allocation during times of scarcity. The authors show that the monoclonal antibody screening score (MASS) and COVID-19 antibody screening tool (CAST) scores can be used to determine clinical priority and guide allocation by identifying subgroups of eligible patients who are most at risk of hospitalization and would benefit the most from casirivimab-imdevimab treatment prioritization.
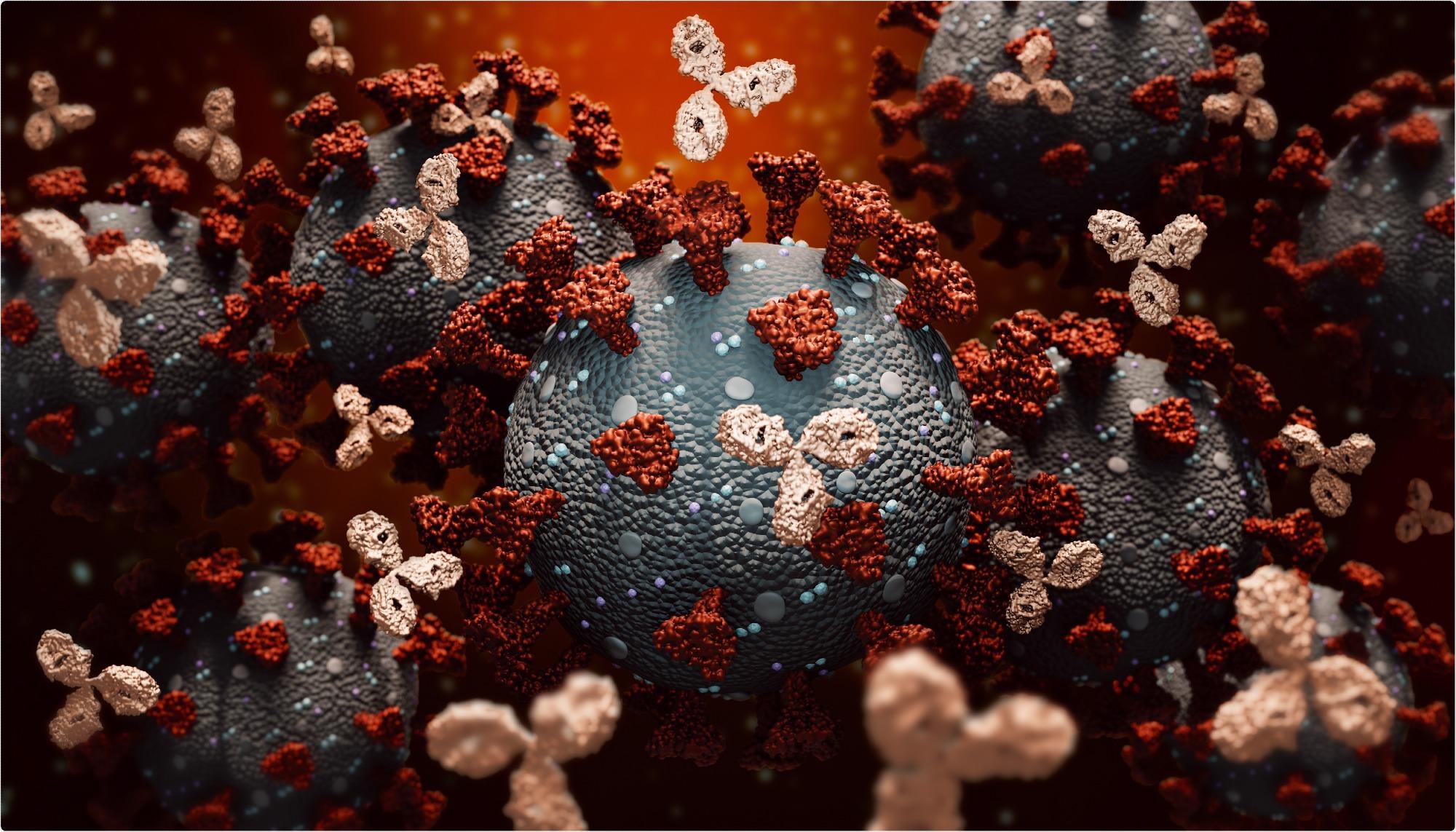 Study: Clinical Prioritization of Antispike Monoclonal Antibody Treatment of Mild to Moderate COVID-19. Image Credit: MattLphotography / Shutterstock
Study: Clinical Prioritization of Antispike Monoclonal Antibody Treatment of Mild to Moderate COVID-19. Image Credit: MattLphotography / Shutterstock
The study
The patients' hospitalization rates rose in direct correlation with CAST and MASS, particularly in those who did not get monoclonal antibodies. A CAST score of 1 or higher is considered more sensitive, but a MASS score of 1 or higher is considered more specific for hospitalization. Patients with a CAST score of 1 are less likely to require COVID-19 hospitalization, according to the authors; the latter group includes patients who were identified using the enhanced emergency use authorization (EUA) criteria adopted in May 2021.
The all-cause and COVID-19 hospitalization rates were 7.8% and 0.1%, respectively, in the population of 218 untreated patients in these strata. Interestingly, two-thirds of all-cause hospitalizations in this cohort were for childbirth. Adjusting for pregnancy results in an all-cause hospitalization rate of only 1.8%, which compares favorably to rates in individuals without any qualifying high-risk condition. As a result, during times of resource scarcity, this group of eligible but lower-risk patients may be given lower priority so that individuals with higher CAST and MASS scores can receive care.
The findings of this study support the authors' previous conclusions, which show a direct link between the number of medical comorbidities and the rate of hospitalization in high-risk patients with mild to moderate COVID-19 since the initiation of MATRx in November 2020. During periods of scarcity, such as during overwhelming surges of SARS-CoV-2 infection in the United States or other countries where anti-spike monoclonal antibody supplies are scarce, people with multiple medical comorbidities (higher MASS and CAST scores) should be given priority for monoclonal antibody allocation.
This technique aims to lower the likelihood of illness development, reducing the potential load on already overburdened healthcare systems. Furthermore, this prioritizing method should also be applied to patients with mild to moderate COVID-19 who are already in the hospital for another reason in order to limit the risk of disease development and the necessity for intensive care unit admission. The authors further suggest that during times of shortage, treatment of high-risk COVID-19 patients should take precedence over postexposure prophylaxis, with the exception of exposed unvaccinated or immunocompromized vital employees.
Patients with mild to severe COVID-19 have a limited time to receive these life-saving monoclonal antibody medicines. Thus they should be prioritized above exposed asymptomatic high-risk individuals who will have a second shot at monoclonal antibody infusion if symptoms emerge. Only if qualified high-risk individuals exhibit symptoms after exposure and are not offered postexposure prophylaxis because of shortages should they be thoroughly followed and treated early.
Because of society's reliance on vital employees, they should be given first priority for postexposure prophylaxis if they are still at risk due to an underlying immunocompromised condition or have not yet received all of their vaccines.
Implications
Monoclonal antibody allocation should be based on patient needs and the likelihood of benefit when resources are limited. MASS and CAST as paired screening methods were proven to be clinically beneficial in accomplishing this goal in this program. The authors recommend Anti-spike monoclonal antibodies as a way to reduce the number of patients admitted to the hospital due to COVID-19-related illnesses and relieve the strain on an already overburdened healthcare system. There should be a serious consideration of these two clinical instruments to guarantee that vital and critical employees and the underserved and underrepresented communities have equal access to anti-spike monoclonal antibodies as the SARS-CoV-2 delta variant surges.