
 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Introduction
The SARS-CoV-2 Omicron variant became the dominant circulating variant of concern (VOC) in the Quebec (QC) province of Canada by December 20, 2021. Simultaneously, there was an increase in the number of HCWs reporting household exposures of confirmed COVID-19 cases due to the high community transmission of the SARS-CoV-2 Omicron variant.
The most recent provincial COVID-19 guidelines regard everyone as unprotected and recommend that SARS-CoV-2-infected HCWs isolate for ten days. Furthermore, all household contacts should quarantine, as studies have demonstrated the loss of two-dose COVID-19 vaccine effectiveness in preventing Omicron infection.
However, the tertiary care mother and child hospital, Centre Hospitalier Universitaire (CHU) Sainte-Justine in QC, Canada, allowed HCWs exposed to confirmed COVID-19 household cases to work if they have received two or more doses of COVID-19 vaccines, were asymptomatic or with symptoms, received a negative reverse transcription-polymerase chain reaction (RT-PCR) test, and followed proper preventive measures due to the potential risk of workforce shortages.
About the study
In the present cohort study, the researchers determined the risk of HCWs exposed to a SARS-CoV-2-positive household contact to become COVID-positive and the risk of nosocomial COVID-19 transmission.
Study participants were HCWs with a history of household exposure to SARS-CoV-2-positive cases who contacted the CHU Sainte-Justine's Occupational Health and Safety (OHS) unit, Montreal (QC) Canada, between December 20, 2021, and January 17, 2022.
The main outcome of the study was a positive RT-PCR test result for SARS-CoV-2. Several data sets were analyzed during the study, including HCW vaccination dates and the number of doses, RT-PCR results and tested dates, symptoms reported by the HCW during the initial test, cases of COVID-19 outbreaks among HCWs, and healthcare-acquired COVID-19 in patients.
The outbreak of SARS-CoV-2 among HCWs and nosocomial COVID-19 among patients were identified through the daily evaluation of Quebec Ministry of Health and Social Services-reported COVID-19 cases as part of the regular Infection Prevention and Control surveillance (IPAC) procedure. Nosocomial SARS-CoV-2 infection was suspected in patients if symptoms occurred three or more days after the hospital admission.
Study findings
Nearly 50% of HCWs with a known SARS-CoV-2-positive household contact remained negative during the study period. Among the HCWs who became positive for SARS-CoV-2, 82.4% tested positive during the initial RT-PCR test and were quarantined.
Out of the 279 HCWs allowed to work despite having a confirmed COVID-19 household contact, nearly 15% became COVID-positive from a median of four days after the initial SARS-CoV-2 screening test.
The household secondary attack rate (SAR) of Omicron in booster-vaccinated individuals was 42%. HCWs without symptoms or those who received booster vaccination more than seven days before the COVID-positive household exposure had an 88% chance of remaining SARS-CoV-2 negative.
Although a total of ten COVID-19 outbreaks occurred among HCWs during the study period, which was defined as three positive HCWs per outbreak, none of these infected individuals was associated with an HCW with COVID-positive household contact. In fact, some outbreaks were associated with a household contact after the contact tracing of the COVID-positive HCW.
Among the nine patients with hospital-acquired COVID-19, six were associated with parents of the children, visitors, and other COVID-positive patients. No source was identified for the remaining three cases.
Taken together, no healthcare-associated SARS-CoV-2 transmission to patients or COVID-19 outbreak among HCWs was observed when an HCW with a known SARS-CoV-2-positive household exposure was allowed to work.
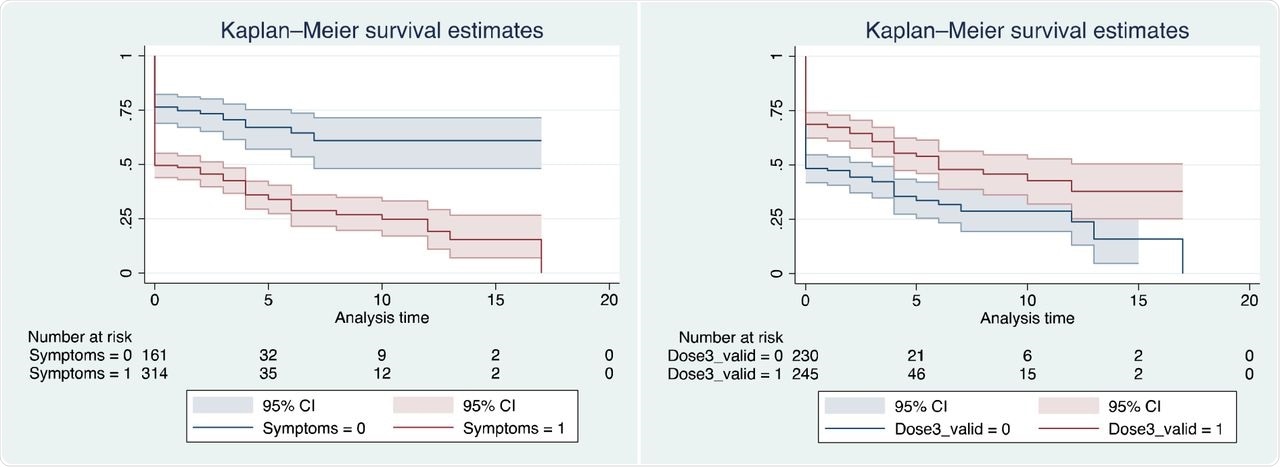
Survival curves for remaining RT-PCR negative (a) stratified by presence of symptoms at first test; (b) stratified by vaccination status.
Conclusions
The present study found a 50% household SAR of Omicron, which was higher than those reported in a previous Danish study. This is likely because of the comprehensive outcome assessment in the present study using the RT-PCR test for diagnosing secondary cases, rather than the rapid-antigen test used in the Danish study.
The authors suggest that measures implemented to reduce nosocomial COVID-19 should be meticulously balanced with the risk of HCW shortage in hospitals. Furthermore, the proper usage of personal protective equipment can efficiently limit SARS-CoV-2 transmission.
Altogether, several factors must be considered while determining the significance of quarantining HCWs with a household exposure of confirmed COVID-19 case. These include the risk of SARS-CoV-2 transmission to HCWs who have a lower risk of complications, given the higher vaccination rates, the probable impact of SARS-CoV-2 transmission to patients in a mother-child care hospital setting, who have a better recovery chance even if infected, and the risk to patients if highly specialized staff shortages occur.
Overall, the study findings demonstrate that considering the consequences of staffing shortages, allowing booster-vaccinated HCWs without SARS-CoV-2 symptoms to work is a safe alternative during the COVID-19 pandemic.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Quach, C., Blanchard, A. C., Lamarche, J., et al. (2022). Should healthcare workers with SARS-CoV-2 household exposures work? A Cohort Study. medRxiv. doi:10.1101/2022.01.23.22269719. https://www.medrxiv.org/content/10.1101/2022.01.23.22269719v1
- Peer reviewed and published scientific report.
Blanchard, Ana C., Valérie Lamarre, Josée Lamarche, Nathalie Audy, and Caroline Quach. 2022. “Mitigating Healthcare Staffing Shortages: Should Healthcare Workers with Severe Acute Respiratory Coronavirus Virus 2 (SARS-CoV-2) Household Exposures Work?” Infection Control & Hospital Epidemiology, August, 1–3. https://doi.org/10.1017/ice.2022.195. https://www.cambridge.org/core/journals/.